Acute Cytitis
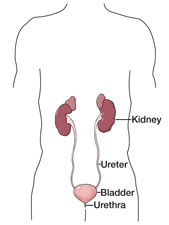
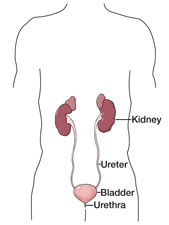
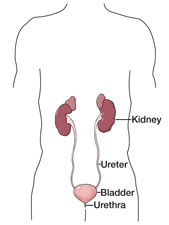 | Your doctor has determined that you have acute cystitis, a form of urinary tract infection (UTI) often referred to as a bladder infection. Each year in the U.S., nearly 10 million people develop a UTI, with women affected much more often than men. The bladder is a stretchable oval chamber in the lower abdomen that is part of the urinary tract, which also includes the kidneys, ureters and urethra. Its main purpose is to store urine. The kidneys remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder. Urine is emptied out of the body from the bladder through the urethra. Acute cystitis — the most common type of UTI — occurs when bacteria enter the opening of the urethra and spread to the bladder. In about 80% of cases, the cause is a type of bacteria called Escherichia coli (E. coli), which are normally present in the digestive tract. Other bacteria that can cause bladder infections include Staphylococcus saprophyticus, Chlamydia trachomatis and Mycoplasma hominis. The bacteria enter the urethral opening from the skin around the anus or genitals in various ways, such as wiping from back to front after using the toilet or having a urinary catheter (tube) placed in the bladder to drain urine from the body. Sexual intercourse can trigger UTIs in some women, as can the use of a diaphragm for birth control. Being pregnant or having certain diseases such as diabetes, HIV, cancer and sickle cell anemia also increases the risk of developing acute cystitis. It is believed that women develop UTIs more often then men because of their shorter urethras, which exit the body closer to the source of bacteria. Although women suffer these infections more frequently, they are often more serious and harder to treat in men. The most common symptoms of acute cystitis include: • Burning or pain when urinating |
It is important to deal with acute cystitis promptly when it develops, as it can progress to a kidney infection if left untreated. Kidney infection is a serious condition that requires immediate treatment and can cause reduced kidney function or even death.
Antibiotics are used to kill the bacteria that cause acute cystitis. The type of drug prescribed and the length of treatment depend on the type of bacteria and other factors such as your age, sex and general health condition. Medications used include amoxicillin, trimethoprim-sulfamethoxazole, fluoroquinolones, tetracycline and doxycycline.
To make sure your infection clears up completely and prevent a kidney infection, you should take your medication as directed and finish the entire supply, even though you may feel better within a couple of days. Your doctor may schedule a follow-up exam to test your urine after treatment is finished to confirm that the bacterial infection is gone.
Some people develop UTIs frequently, three or more times each year. In those cases, low-dose antibiotics may be prescribed for six months or longer to prevent repeat infections. Scientists are working to develop a vaccine to prevent UTIs that may be taken as a pill or vaginal suppository.
To help reduce symptoms of acute cystitis, you should drink plenty of water and avoid coffee, alcohol and smoking. You can use a heating pad on your lower abdomen and take an over-the-counter (OTC) pain medication containing ibuprofen or acetaminophen to ease the pain, as well as sit in a shallow tub of hot water to help with burning of the urethral opening.
In addition, you may want to take the OTC medication phenazopyridine for pain relief. Although you will feel a masking of symptoms with this drug, it is important to remember that is not an antibiotic and it will not cure your infection. Be sure to follow the package instructions carefully, and talk with your doctor about what prescription and OTC medications are best for your individual situation.
Steps you can take to prevent future UTIs include:
• Drinking at least 6–8 glasses of liquids each day, preferably water
• Urinating frequently and going when you first feel the urge
• Taking showers instead of baths and avoiding bubble bath during a tub bath
• Wiping from front to back after using the toilet, especially after bowel movements
• Drinking cranberry or blueberry juice sweetened with fruit juice (rather than sugar)
• Avoiding scented toilet paper and feminine products
• Wearing cotton underwear and avoiding tight-fitting jeans and nylon underwear
• Cleansing the genital area before sexual intercourse and urinating afterward
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
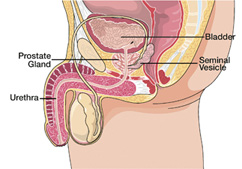
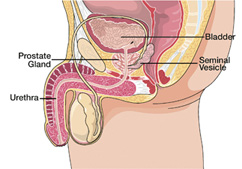
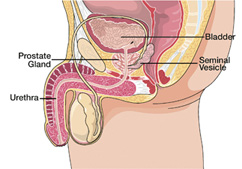
Benign Prostatic Hyperplasia
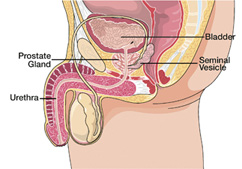 | Your doctor has determined that you have benign prostatic hyperplasia, or BPH, a normal enlargement of the prostate gland that occurs in men as they get older. BPH is not cancer and does not increase the risk of developing prostate cancer. The chance of developing BPH increases with age. More than half of all men over the age of 60, and about 90% of those over age 70, have symptoms of the condition. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Benign prostatic hyperplasia occurs when the prostate grows in size as a man gets older. The exact cause of this normal prostate enlargement is still the subject of research, but it seems to be related to the hormonal changes of aging. The prostate is encased in a layer of tissue and does not expand outwardly as it enlarges. The gland instead pushes inward against the urethra, which can cause a partial, or sometimes complete, blockage. In response to the blockage, the wall of the bladder thickens and becomes irritable. The bladder will then contract more forcefully, even when only slightly full, to push urine through the narrowed urethra. The result is a need to urinate frequently, especially at night. Other symptoms caused by BPH include: • Suddenly and urgently needing to urinate Not all men with BPH suffer the troublesome urinary symptoms that can arise from the condition. |
BPH only needs treatment if the symptoms are particularly bothersome or if the urinary tract is seriously affected. Deciding on a treatment plan can depend upon a variety of factors, such as the severity of the condition and your age, general health condition and personal preferences. The following treatment possibilities are available:
Watchful Waiting – Some patients with mild symptoms decide not to pursue active therapy for their BPH, but rather adopt a “wait and watch” tactic. Men who choose this approach usually have an annual exam to check the status of their condition. If troublesome symptoms develop, a plan of treatment can be implemented.
Medication – BPH can be treated with medications that help relax prostate gland muscles (alpha blockers), drugs that help the prostate to shrink (5-alpha reductase inhibitors) or a combination of the two. These drugs improve urinary flow and symptoms, and are taken orally every day.
Surgery – Three main types of surgery are used to treat BPH: transurethral resection of the prostate (TURP), transurethral incision of the prostate (TUIP) and prostatectomy. TURP is the most common BPH surgery and helps relieve symptoms in men who have trouble urinating. During the procedure, prostate tissue that blocks urine flow is removed. During the TUIP procedure, one or two small cuts are made in the prostate to reduce pressure on the urethra, making urinating easier. Prostatectomy is the removal of part or all of the prostate gland.
Other Treatments – Additional treatments for BPH include laser surgery and thermal therapy (with microwave or radiofrequency energy) to destroy prostate tissue, as well as prostatic stents, which are spring-like devices placed in the urethra to hold it open.
To help reduce the symptoms of BPH, you can:
• Employ hydrotherapy up to three times each day by sitting in a tub of cold water for 15–30 minutes
• Use cold packs applied between the scrotum and anus
• Avoid sugar, caffeine, dairy products, alcohol (especially beer), and fried and refined foods
• Drink plenty of water and eat healthy foods such as fruits and vegetables, whole grains, beans, soy, seeds and nuts, olive oil and cold-water fish (e.g., salmon, tuna, halibut, mackerel)
• Avoid over-the-counter antihistamines and decongestants, which can make it more difficult to urinate
• Take dietary supplements or herbs such as zinc, flaxseed meal, beta-sitosterol, flower pollen, saw palmetto or stinging nettles
Be sure to consult your doctor before taking any supplements or herbs.
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
The Prostatitis Foundation, 888. 891.4200, http://www.prostatitis.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Biopsy Suspicious for Prostate Cancer
 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of biopsy suspicious for prostate cancer. This means that the cells from your prostate gland do not fully look like cancer, but they also do not look like normal prostate cells. Men diagnosed with suspicious prostate biopsies are at considerable risk of later being diagnosed with prostate cancer. In one study, some 38% of patients with suspicious biopsies were diagnosed with prostate cancer after follow-up biopsies were taken within six weeks of the original diagnosis. Because cancer may be present elsewhere in the prostate gland for men with suspicious biopsies, the most recommended course of action is to schedule a repeat prostate biopsy soon after the initial diagnosis. You should talk with your doctor about this possibility. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. |
You can choose to take an active role in your health and well-being. Since it is possible that you may have prostate cancer, you should learn as much as you can about the condition. Have a list of questions ready each time you meet with your doctor, and be sure to report any new symptoms if they arise. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Bladder Cancer
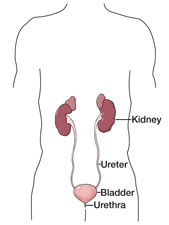
 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of bladder cancer, or cancer that begins in the bladder. Bladder cancer occurs more than twice as often in men than women, and most frequently in Caucasians. The risk of developing the condition increases greatly with age, especially after the age of 55. The bladder is a stretchable oval chamber in the lower abdomen that is part of the urinary tract, which also includes the kidneys, ureters and urethra. Its main purpose is to store urine. The kidneys remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder. Urine is emptied out of the body from the bladder through the urethra. Cancer occurs when cells in the bladder have lost the ability to develop and die in their normal manner. These abnormal cells form a growth, or tumor, which can be benign (non-cancerous) or malignant (cancerous). Benign tumors do not have the ability to spread to other sites in the body (metastasize). Bladder cancer cells, however, have the potential to invade locally through the bladder wall or to metastasize. More than 90% of bladder cancers form from the lining of the bladder (urothelium) and are called urothelial cell carcinoma. Exposure to cancer-causing agents (carcinogens) contributes to the growth of bladder cancer including cigarette smoke, which is estimated to cause about half of all cases. Other risk factors include working in certain industries and having chronic bladder infections, urinary stones or a family history of bladder cancer. Your doctor may want to perform one or more tests to see if the cancer has spread, such as a CT scan, intravenous pyelogram, cystoscopy, biopsy, MRI scan, ultrasound, X-ray or bone scan. Cancer that is confined within the bladder wall is the most manageable and curable. If malignant cells extend through the bladder wall into surrounding tissues, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable bladder cancer to help minimize pain and improve quality of life. Talk with your doctor about your specific stage of cancer. |
Deciding on a treatment plan for your bladder cancer can be complex and depend upon a variety of factors, such as your age, general health condition, stage of cancer and personal preferences. Sometimes more than one type of therapy may be used. The following treatment possibilities are available:
Surgery – Three main surgical procedures are used to treat bladder cancer: transurethral resection, partial cystectomy and radical cystectomy. Transurethral resection to remove the tumor is performed only for early stage cancers and involves the use of a camera (cystoscope) inserted through the urethra. In partial cystectomy, a portion of the bladder is removed. In cases where the cancer has invaded deeply into the bladder wall, a radical cystectomy may be performed, which removes the entire bladder and nearby lymph nodes. In rare cases, more extensive surgery may be required. During surgery it may be necessary to create a urostomy to allow urine to leave the body through the abdominal wall to be collected in a bag. However, newer surgical methods make it possible to create an internal pouch for urine collection in some cases.
Radiation Therapy – Another treatment method for bladder cancer is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy destroys cancer cells with small implants that are placed directly into the tumor. Radiation therapy can also help reduce symptoms in advanced bladder cancer.
Chemotherapy – Anti-cancer drugs, or chemotherapy, are often administered to treat bladder cancer. One particular method called intravesical chemotherapy is used to treat early stage bladder cancer. It involves placing chemotherapy drugs directly into the bladder via a catheter inserted in the urethra. Chemotherapy is often administered shortly before or after surgery.
Biologic Therapy – A newer treatment option called biologic therapy is used to enhance the immune system’s ability to destroy malignant cells. Intravesical biologic therapy delivers bacillus Calmette-Guerin (BCG) solution directly into the bladder through the urethra to treat early stage bladder cancer.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep every night.
In addition you should report any new symptoms promptly to your doctor, who will likely recommend periodic exams and testing to monitor your health since bladder cancer has a high recurrence rate.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
Chronic Cystitis
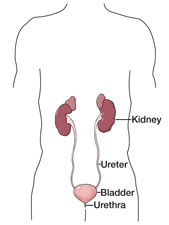
 | Your doctor has determined that you have chronic cystitis, a repeated or prolonged form of urinary tract infection (UTI) that causes inflammation of the bladder. The bladder is a stretchable oval chamber in the lower abdomen that is part of the urinary tract, which also includes the kidneys, ureters and urethra. Its main purpose is to store urine. The kidneys remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder. Urine is emptied out of the body from the bladder through the urethra. Cystitis is an infection caused by bacteria that enter the opening of the urethra and spread to the bladder. Chronic, or persistent, cystitis occurs when a patient does not respond to the usual treatment for cystitis, has a case that lasts longer than two weeks, or has repeated cases of infection more than twice in a six-month span. In non-chronic, or acute, cases of cystitis, symptoms normally improve within two days after treatment begins. The bacteria that cause cystitis enter the urethral opening from the skin around the anus or genitals in various ways, such as wiping from back to front after using the toilet or having a urinary catheter (tube) placed in the bladder to drain urine from the body. Sexual intercourse can trigger UTIs in some women, as can the use of a diaphragm for birth control. Being pregnant or having certain diseases such as diabetes, HIV, cancer and sickle cell anemia also increases the risk of developing cystitis, as does having urinary tract abnormalities or blockages or prostate enlargement (benign prostatic hyperplasia). The most common symptoms of chronic cystitis include burning or pain when urinating, a feeling of pressure in the lower abdomen, cloudy, bloody or odd-smelling urine, frequent and sometimes intense urges to urinate, fever and general discomfort, lower back or abdominal pain and an inability to urinate despite the urge to go. Other symptoms may include incontinence (involuntary loss of urine), nausea and vomiting, and mental changes or confusion in the elderly. |
Chronic cystitis should be treated thoroughly because it can progress to a kidney infection if left untreated. Kidney infection is a serious condition that requires immediate treatment and can cause reduced kidney function or even death. Chronic cystitis can also cause sepsis, a severe and often life-threatening illness marked by a bacterial infection of the bloodstream.
Antibiotics are used to kill the bacteria that cause cystitis. The type of drug prescribed and the length of treatment depend on the type of bacteria and other factors such as your age, sex and general health condition. Medications used include amoxicillin, trimethoprim-sulfamethoxazole, fluoroquinolones, tetracycline, nitrofurantoin and doxycycline. Frequently, low-dose antibiotics may be prescribed for six months to two years to prevent repeat infections. In some cases, physicians recommend single antibiotic doses to be taken after sexual intercourse as a preventive measure.
To make sure your infection clears up completely and prevent a kidney infection, you should take your medication as directed and finish the entire supply, even though you may feel better before you have completed your prescription. If a urinary tract abnormality is causing the chronic cystitis, corrective surgery may also be needed.
Your doctor may schedule a follow-up exam to test your urine after treatment is finished to confirm that the bacterial infection is gone. Be sure to call your doctor if your symptoms worsen or you develop additional symptoms.
To help reduce symptoms of chronic cystitis, you should drink plenty of water and avoid coffee and other caffeinated drinks, citrus juices, spicy foods, alcohol and smoking. You can use a heating pad on your lower abdomen and take an over-the-counter (OTC) pain medication containing ibuprofen or acetaminophen to ease the pain, as well as sit in a shallow tub of hot water to help with burning of the urethral opening.
In addition, you may want to take the OTC medication phenazopyridine for pain relief. Although you will feel a masking of symptoms with this drug, it is important to remember that is not an antibiotic and it will not cure your infection. Be sure to follow the package instructions carefully, and talk with your doctor about what prescription and OTC medications are best for your individual situation.
Steps you can take to prevent future UTIs include:
• Drinking at least 6–8 glasses of liquids each day, preferably water
• Urinating frequently and going when you first feel the urge
• Taking showers instead of baths and avoiding bubble bath during a tub bath
• Wiping from front to back after using the toilet, especially after bowel movements
• Drinking cranberry or blueberry juice sweetened with fruit juice (rather than sugar)
• Avoiding scented toilet paper and feminine products
• Wearing cotton underwear and avoiding tight-fitting jeans and nylon underwear
• Cleansing the genital area before sexual intercourse and urinating afterward
• Making sure your urinary catheter is changed or cleaned often if you use one
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
Kidney Stones
Your doctor has determined that you have one or more kidney stones, one of the most common disorders of the urinary tract. Your particular type of kidney stone is called a calcium stone, which occurs in about 80% of all kidney stone cases. Nearly 1 million Americans are treated for kidney stones each year, with men developing the condition about four times more often than women.
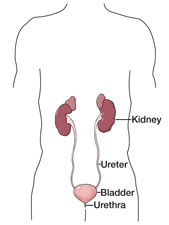
 The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
Kidney stones occur when certain minerals and other chemicals in the urine form crystals that bind together in a hard mass. They may range in size from a grain of sand to a golf ball and can be either smooth or jagged.
There are four different types of kidney stones, each containing specific chemical and mineral combinations. The most common type is made of calcium combined with oxalate or phosphate. Other kidney stone types include struvite stones, which are caused by urinary tract infection, uric acid stones and cystine stones, which are made of the amino acid cystine.
Kidney stones often cause severe pain, especially when they block urine flow; however, they can be present without causing symptoms. These “silent” stones are often discovered on X-rays.
Deciding on a treatment plan for your kidney stones can depend upon a variety of factors such as their type, location and size. The following treatment possibilities are available:
Watchful Waiting – About 90% of kidney stones pass through the urinary system on their own within a short period of time, especially when 2–3 quarts of water is consumed daily to help move them along. This process often takes place at home, with pain medication prescribed as needed. Patients are often asked to collect the stones so their composition can be analyzed by a laboratory.
Medication – Some types of kidney stones may be dissolved using medications; however, calcium-based stones cannot be treated by this method. Drugs such as diuretics, citrates, phosphates and cholestyramine can be used to prevent more stones from forming.
Extracorporeal Shockwave Lithotripsy – The most often used treatment procedure for kidney stones is extracorporeal shockwave lithotripsy (ESWL), which is usually done on an outpatient basis and has a short recovery period. ESWL uses shock waves created outside the body to focus on and disintegrate the stones. The waves are harmless to the skin and other tissues, and break down kidney stones into sand-like fragments that are easily passed in the urine.
Percutaneous Nephrolithotomy – When a kidney stone is very large or in a location that prohibits the use of ESWL, a procedure called percutaneous nephrolithotomy is often performed. It involves making a very small incision in the back and inserting a camera (nephroscope) into the kidney to see and remove the stone. An energy probe (ultrasonic or electrohydraulic) may be required to break larger stones into pieces before they can be removed.
Ureteroscopic Removal – In cases when kidney stones are located in the middle or lower ureter, ureteroscopy may be necessary. This procedure is performed using a small fiber-optic camera (ureteroscope) passed through the urethra and bladder into the ureter to see and remove the stone. A small, cage-like device captures the stone for removal, or it can be shattered with a shock wave into smaller pieces if needed.
In very rare cases, invasive open surgery, called nephrolithotomy, may need to be performed.
People who have had more than one kidney stone or with a family history of the condition are likely to develop more stones. You can help prevent new kidney stones. One of the key steps is to drink more liquids throughout each day and night — a minimum of 10 full glasses — with at least half being water. Because you have calcium kidney stones, your doctor may also suggest that you do one or more of the following:
• Limit your intake of sodium
• Maintain normal to high levels of dietary calcium (milk, cheese, etc.)
• Consume meat, seafood and poultry in moderation
• Limit your intake of beets, coffee, tea, cola, cocoa and chocolate, pepper, nuts, spinach, rhubarb, strawberries, wheat bran and grapefruit juice
• Take daily vitamin B6 supplements
Depending on your urine chemistry, your doctor may also suggest that you avoid eating foods with added vitamin D and taking calcium-based antacids and vitamin C supplements. You may also be advised to use calcium citrate supplements, drink lemon juice and eat a low-fat diet. Be sure to talk with your doctor about what specific dietary changes, medications and supplements are best for your individual situation.
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Kidney Foundation, 800.622.9010, http://www.kidney.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
Your doctor has determined that you have one or more kidney stones, one of the most common disorders of the urinary tract. Your particular type of kidney stone is called a cystine stone, which occurs in about 2% of all kidney stone cases. Nearly 1 million Americans are treated for kidney stones each year, with men developing the condition about four times more often than women.
 The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
Kidney stones occur when certain minerals and other chemicals in the urine form crystals that bind together in a hard mass. They may range in size from a grain of sand to a golf ball and can be either smooth or jagged.
There are four different types of kidney stones, each containing specific chemical and mineral combinations. The most common type is made of calcium combined with oxalate or phosphate. Other kidney stone types include struvite stones, which are caused by urinary tract infection, uric acid stones and cystine stones, which are made of the amino acid cystine.
Kidney stones often cause severe pain, especially when they block urine flow; however, they can be present without causing symptoms. These “silent” stones are often discovered on X-rays.
Deciding on a treatment plan for your kidney stones can depend upon a variety of factors such as their type, location and size. The following treatment possibilities are available:
Watchful Waiting – About 90% of kidney stones pass through the urinary system on their own within a short period of time, especially when 2–3 quarts of water is consumed daily to help move them along. This process often takes place at home, with pain medication prescribed as needed. Patients are often asked to collect the stones so their composition can be analyzed by a laboratory.
Medication – Some types of kidney stones may be dissolved using medications. Drugs such as tiopronine and penicillamine are sometimes used to reduce the amount of cystine in the urine, which can prevent more stones from forming.
Extracorporeal Shockwave Lithotripsy – The most often used treatment procedure for kidney stones is extracorporeal shockwave lithotripsy (ESWL), which is usually done on an outpatient basis and has a short recovery period. ESWL uses shock waves created outside the body to focus on and disintegrate the stones. The waves are harmless to the skin and other tissues, and break down kidney stones into sand-like fragments that are easily passed in the urine.
Percutaneous Nephrolithotomy – When a kidney stone is very large or in a location that prohibits the use of ESWL, a procedure called percutaneous nephrolithotomy is often performed. It involves making a very small incision in the back and inserting a camera (nephroscope) into the kidney to see and remove the stone. An energy probe (ultrasonic or electrohydraulic) may be required to break larger stones into pieces before they can be removed.
Ureteroscopic Removal – In cases when kidney stones are located in the middle or lower ureter, ureteroscopy may be necessary. This procedure is performed using a small fiber-optic camera (ureteroscope) passed through the urethra and bladder into the ureter to see and remove the stone. A small, cage-like device captures the stone for removal, or it can be shattered with a shock wave into smaller pieces if needed.
In very rare cases, invasive open surgery, called nephrolithotomy, may need to be performed.
People who have had more than one kidney stone or with a family history of the condition are likely to develop more stones. You can help prevent new kidney stones. One of the key steps is to drink a high volume of water throughout each day and night — a minimum of a gallon. A third of the water should be consumed during the night. Because you have cystine kidney stones, your doctor may also suggest that you do one or more of the following:
• Eat more fruits and vegetables
• Consume meat, seafood and poultry in moderation
• Increase the pH of your urine by taking sodium bicarbonate
Be sure to talk with your doctor about what specific dietary changes, supplements and medications are best for your individual situation.
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Kidney Foundation, 800.622.9010, http://www.kidney.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
Your doctor has determined that you have one or more kidney stones, one of the most common disorders of the urinary tract. Your particular type of kidney stone is called a struvite stone, which occurs in about 9% of all kidney stone cases. Nearly 1 million Americans are treated for kidney stones each year, with men developing the condition about four times more often than women.
 The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
Kidney stones occur when certain minerals and other chemicals in the urine form crystals that bind together in a hard mass. They may range in size from a grain of sand to a golf ball and can be either smooth or jagged.
There are four different types of kidney stones, each containing specific chemical and mineral combinations. The most common type is made of calcium combined with oxalate or phosphate. Other kidney stone types include struvite stones, which are caused by urinary tract infection, uric acid stones and cystine stones, which are made of the amino acid cystine.
Kidney stones often cause severe pain, especially when they block urine flow; however, they can be present without causing symptoms. These “silent” stones are often discovered on X-rays.
Deciding on a treatment plan for your kidney stones can depend upon a variety of factors such as their type, location and size. The following treatment possibilities are available:
Watchful Waiting – About 90% of kidney stones pass through the urinary system on their own within a short period of time, especially when 2–3 quarts of water is consumed daily to help move them along. This process often takes place at home, with pain medication prescribed as needed. Patients are often asked to collect the stones so their composition can be analyzed by a laboratory.
Medication – Struvite stones may be dissolved through urinary tract irrigation with a solution of organic acids. In some cases the drug acetohydroxamic acid is prescribed along with long-term antibiotics, or an aluminum hydroxide gel is administered to prevent more stones from forming.
Extracorporeal Shockwave Lithotripsy – The most often used treatment procedure for kidney stones is extracorporeal shockwave lithotripsy (ESWL), which is usually done on an outpatient basis and has a short recovery period. ESWL uses shock waves created outside the body to focus on and disintegrate the stones. The waves are harmless to the skin and other tissues, and break down kidney stones into sand-like fragments that are easily passed in the urine.
Percutaneous Nephrolithotomy – When a kidney stone is very large or in a location that prohibits the use of ESWL, a procedure called percutaneous nephrolithotomy is often performed. It involves making a very small incision in the back and inserting a camera (nephroscope) into the kidney to see and remove the stone. An energy probe (ultrasonic or electrohydraulic) may be required to break larger stones into pieces before they can be removed.
Ureteroscopic Removal – In cases when kidney stones are located in the middle or lower ureter, ureteroscopy may be necessary. This procedure is performed using a small fiber-optic camera (ureteroscope) passed through the urethra and bladder into the ureter to see and remove the stone. A small, cage-like device captures the stone for removal, or it can be shattered with a shock wave into smaller pieces if needed.
In very rare cases, invasive open surgery, called nephrolithotomy, may need to be performed.
People who have had more than one kidney stone or with a family history of the condition are likely to develop more stones. You can help prevent new kidney stones. One of the key steps is to drink more liquids throughout each day and night — a minimum of 10 full glasses — with at least half being water. Because you have struvite kidney stones, your doctor may also suggest that you do one or more of the following:
• Drink cranberry juice
• Consume meat, seafood and poultry in moderation
• Test your urine for acidity and bacteria
Be sure to talk with your doctor about what specific dietary changes, supplements and medications are best for your individual situation.
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Kidney Foundation, 800.622.9010, http://www.kidney.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
Your doctor has determined that you have one or more kidney stones, one of the most common disorders of the urinary tract. Your particular type of kidney stone is called a uric acid stone, which occurs in about 9% of all kidney stone cases. Nearly 1 million Americans are treated for kidney stones each year, with men developing the condition about four times more often than women.
 The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
The kidneys are two bean-shaped organs located toward the middle of the back that are part of the urinary tract, which also includes the ureters, bladder and urethra. Their main purpose is to remove extra water and wastes from the blood and convert them to urine. The ureters are narrow tubes that transport urine from the kidneys to the bladder, a stretchable oval chamber in the lower abdomen. Urine is emptied out of the body from the bladder through the urethra.
Kidney stones occur when certain minerals and other chemicals in the urine form crystals that bind together in a hard mass. They may range in size from a grain of sand to a golf ball and can be either smooth or jagged.
There are four different types of kidney stones, each containing specific chemical and mineral combinations. The most common type is made of calcium combined with oxalate or phosphate. Other kidney stone types include struvite stones, which are caused by urinary tract infection, uric acid stones and cystine stones, which are made of the amino acid cystine.
Kidney stones often cause severe pain, especially when they block urine flow; however, they can be present without causing symptoms. These “silent” stones are often discovered on X-rays.
Deciding on a treatment plan for your kidney stones can depend upon a variety of factors such as their type, location and size. The following treatment possibilities are available:
Watchful Waiting – About 90% of kidney stones pass through the urinary system on their own within a short period of time, especially when 2–3 quarts of water is consumed daily to help move them along. This process often takes place at home, with pain medication prescribed as needed. Patients are often asked to collect the stones so their composition can be analyzed by a laboratory.
Medication – Some types of kidney stones may be dissolved using medications. Drugs such as allopurinol can be used to prevent more stones from forming. In addition, patients with uric acid stones may be advised to take sodium bicarbonate or potassium citrate to hinder stone formation.
Extracorporeal Shockwave Lithotripsy – The most often used treatment procedure for kidney stones is extracorporeal shockwave lithotripsy (ESWL), which is usually done on an outpatient basis and has a short recovery period. ESWL uses shock waves created outside the body to focus on and disintegrate the stones. The waves are harmless to the skin and other tissues, and break down kidney stones into sand-like fragments that are easily passed in the urine.
Percutaneous Nephrolithotomy – When a kidney stone is very large or in a location that prohibits the use of ESWL, a procedure called percutaneous nephrolithotomy is often performed. It involves making a very small incision in the back and inserting a camera (nephroscope) into the kidney to see and remove the stone. An energy probe (ultrasonic or electrohydraulic) may be required to break larger stones into pieces before they can be removed.
Ureteroscopic Removal – In cases when kidney stones are located in the middle or lower ureter, ureteroscopy may be necessary. This procedure is performed using a small fiber-optic camera (ureteroscope) passed through the urethra and bladder into the ureter to see and remove the stone. A small, cage-like device captures the stone for removal, or it can be shattered with a shock wave into smaller pieces if needed.
In very rare cases, invasive open surgery, called nephrolithotomy, may need to be performed.
People who have had more than one kidney stone or with a family history of the condition are likely to develop more stones. You can help prevent new kidney stones. One of the key steps is to drink more liquids throughout each day and night — a minimum of 10 full glasses — with at least half being water. Because you have uric acid kidney stones, your doctor may also suggest that you do one or more of the following:
• Consume meat, seafood and poultry in moderation
• Eat more fruits and vegetables
• Reduce your intake of alcohol, yeast, dried beans and peas, mushrooms, spinach, asparagus and cauliflower
• Test your urine for acidity
Be sure to talk with your doctor about what specific dietary changes, supplements and medications are best for your individual situation.
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Kidney Foundation, 800.622.9010, http://www.kidney.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 3.08
Normal Prostate Biopsy
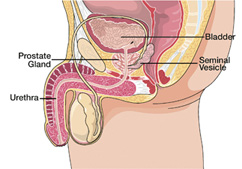 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported finding a normal prostate biopsy. This means that there is no evidence of cancer in your prostate gland. To monitor your urologic health on an ongoing basis, your doctor may recommend annual cancer screenings that include a manual prostate check and blood test. The American Cancer Society endorses such screenings for men age 50 and older who have no serious medical problems, those age 45 and older who are at high risk for developing prostate cancer, and even younger men who have very high risk factors. Men considered at high risk for prostate cancer include African-Americans and those with a family history of the condition, especially in a father or brother. If a man has several close relatives who developed the condition at an early age, he is considered at very high risk. However, no one truly knows why some men develop prostate cancer and others do not. Prostate cancer screenings check the health of the prostate gland, which is typically the size of a walnut and located below the bladder and in front of the rectum in men. The prostate surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Prostate cancer is the second most common cancer in men after skin cancer. |
Chronic cystitis should be treated thoroughly because it can progress to a kidney infection if left untreated. Kidney infection is a serious condition that requires immediate treatment and can cause reduced kidney function or even death. Chronic cystitis can also cause sepsis, a severe and often life-threatening illness marked by a bacterial infection of the bloodstream.
Antibiotics are used to kill the bacteria that cause cystitis. The type of drug prescribed and the length of treatment depend on the type of bacteria and other factors such as your age, sex and general health condition. Medications used include amoxicillin, trimethoprim-sulfamethoxazole, fluoroquinolones, tetracycline, nitrofurantoin and doxycycline. Frequently, low-dose antibiotics may be prescribed for six months to two years to prevent repeat infections. In some cases, physicians recommend single antibiotic doses to be taken after sexual intercourse as a preventive measure.
To make sure your infection clears up completely and prevent a kidney infection, you should take your medication as directed and finish the entire supply, even though you may feel better before you have completed your prescription. If a urinary tract abnormality is causing the chronic cystitis, corrective surgery may also be needed.
Your doctor may schedule a follow-up exam to test your urine after treatment is finished to confirm that the bacterial infection is gone. Be sure to call your doctor if your symptoms worsen or you develop additional symptoms.
Because dietary factors have been associated with the development of prostate cancer, you should keep your diet high in fruits, vegetables and fiber and low in fat, especially animal fat. You may also want to boost your consumption of tomato products such as salsa, ketchup and tomato paste or sauce. Studies have shown that men who eat these foods are less likely to develop prostate cancer because tomatoes contain lycopene, a powerful antioxidant that helps prevent cell damage.
Further steps to help prevent prostate or other types of cancer include:
• Burning up all of the calories you take in each day through healthy eating and regular exercise
• Minimizing stress by getting enough sleep every night and using relaxation techniques
• Cutting out the use of tobacco and limiting your alcohol consumption
• Visiting your doctor regularly and promptly reporting any new symptoms that develop
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Normal TURP Specimen
 | After completing a thorough lab analysis of the tissue samples removed during your recent transurethral resection of the prostate (TURP) procedure, a specialized doctor called a pathologist reported finding a normal TURP specimen. This means that there is no evidence of cancer in your prostate gland. To monitor your urologic health on an ongoing basis, your doctor may recommend annual cancer screenings that include a manual prostate check and blood test. The American Cancer Society endorses such screenings for men age 50 and older who have no serious medical problems, those age 45 and older who are at high risk for developing prostate cancer, and even younger men who have very high risk factors. Men considered at high risk for prostate cancer include African-Americans and those with a family history of the condition, especially in a father or brother. If a man has several close relatives who developed the condition at an early age, he is considered at very high risk. However, no one truly knows why some men develop prostate cancer and others do not. Prostate cancer screenings check the health of the prostate gland, which is typically the size of a walnut and located below the bladder and in front of the rectum in men. The prostate surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Prostate cancer is the second most common cancer in men after skin cancer. |
Because dietary factors have been associated with the development of prostate cancer, you should keep your diet high in fruits, vegetables and fiber and low in fat, especially animal fat. You may also want to boost your consumption of tomato products such as salsa, ketchup and tomato paste or sauce. Studies have shown that men who eat these foods are less likely to develop prostate cancer because tomatoes contain lycopene, a powerful antioxidant that helps prevent cell damage.
Further steps to help prevent prostate or other types of cancer include:
• Burning up all of the calories you take in each day through healthy eating and regular exercise
• Minimizing stress by getting enough sleep every night and using relaxation techniques
• Cutting out the use of tobacco and limiting your alcohol consumption
• Visiting your doctor regularly and promptly reporting any new symptoms that develop
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Prostate Cancer
 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of ductal prostate cancer. This rare type of cancer happens in less than 1% of all prostate cancer cases. Ductal prostate cancer tends to occur in older men. It involves the urethra, or tube that carries urine from the bladder out of the body, and suburethral areas of the prostate. Men with ductal prostate cancer often have an advanced stage of the disease when it is diagnosed.
The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men, surrounding a portion of the urethra. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. While the standard form of prostate cancer usually grows at a slow pace, ductal prostate cancer typically develops and metastasizes quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your age, general health condition, stage of cancer and personal preferences. The following treatment possibilities are available:
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed. Ductal prostate cancer is more likely to recur after surgery than the standard form of the disease.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production. Ductal prostate cancer is generally less likely to respond to hormone therapy than the typical form of the disease.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 2. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Cancer that is located only within the prostate gland is the most manageable and curable. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan |
Deciding on a treatment plan can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer.
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 3. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Cancer that is located only within the prostate gland is the most manageable and curable. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan |
Deciding on a treatment plan can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer.
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 4. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer.
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
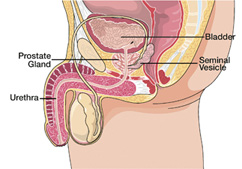 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 5. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed during the procedure.
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
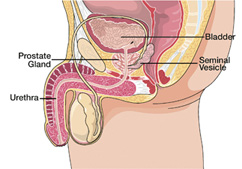 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 6. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed during the procedure.
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
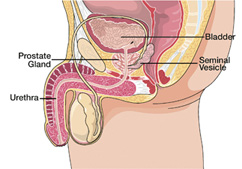 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 7. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed during the procedure.
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
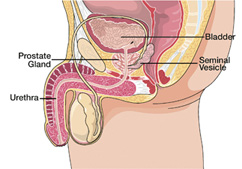 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 8. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed during the procedure.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
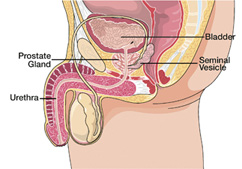 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 9. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed during the procedure.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
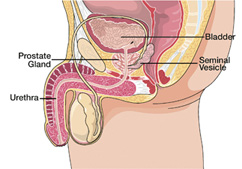 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostate cancer, Gleason score 10. To determine how fast the cancer may grow and spread, your cells were compared to normal prostate cells using the Gleason system, the most common prostate cancer grading method. Gleason scores range from 2 to 10. Gleason scores 2 to 4 designate the least aggressive cancers. Intermediate-grade cancers have Gleason scores of 5 and 6 and can be either slow- or fast-growing. Gleason score 7 indicates moderately aggressive cancer. Cancers with Gleason scores of 8 to 10 are highly aggressive. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. Prostate cancer usually grows at a slow pace, but the most aggressive types can develop and metastasize quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your Gleason score, age, general health condition and personal preferences. The following treatment possibilities are available for prostate cancer:
Watchful Waiting – Some patients decide not to pursue active therapy for their cancer, but rather adopt a “watch and wait” tactic. This choice is often appropriate for older men with small, low-grade tumors that are confined to the prostate. By taking this approach, the side effects of standard prostate cancer treatments are avoided.
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed during the procedure.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
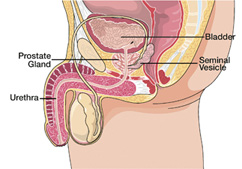 | Your doctor has determined that you have recurrent prostate cancer, which is the return of cancer that was thought to be in remission (not active) or cured. This happens when malignant cells survive in the body after a patient has treatment to remove or destroy cancer. The surviving cells may eventually develop into tumors that become large enough to detect and identify as a recurrence. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Prostate cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a malignant growth, or tumor, which may invade and damage surrounding areas or spread to other locations in the body (metastasize). Recurrent prostate cancer occurs when malignant cells of the same type as the original tumor are found in the body again. These recurrences are categorized as local, regional or distant. A local recurrence of prostate cancer means the malignancy is confined to same area of the body as the original cancer, or very close to it. This can happen even if a patient had a previous surgery to remove the prostate gland. A regional recurrence also involves the same area as the original prostate cancer, but includes nearby lymph nodes or tissues. When prostate cancer recurs at a distance, this means that it has metastasized to other parts of the body. To determine the extent of your cancer is and if it has spread, your doctor may want to perform one or more tests, which could include the following: • MRI Scan Recurrent cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life |
Deciding on a treatment plan for your recurrent prostate cancer can be complex and depend upon a variety of factors, such as your age, general health condition, stage of cancer, previous cancer treatments and personal preferences. Generally, any type of therapy you had before will not be an option. The following treatment possibilities are available:
Surgery – Removal of the entire prostate gland, called radical prostatectomy, is a common way to treat prostate cancer. Surrounding tissues and nearby lymph nodes may also be removed. This procedure can be an option for some patients who previously had radiation therapy.
Cryosurgery – One option for patients with localized cancer is cryosurgery, which uses super-cooled gas to freeze and kill prostate cancer cells.
Radiation Therapy – Another common prostate cancer treatment is radiation therapy, which can be delivered externally or internally. In external beam radiation, a high energy X-ray machine is used to direct radiation at the tumor. Internal radiation therapy, or brachytherapy, destroys cancer cells with small radioactive pellets that are implanted directly into the prostate. Radiation therapy may be helpful for men who previously had a radical prostatectomy.
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production. For patients whose cancer has metastasized, hormone therapy may be the most effective treatment.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
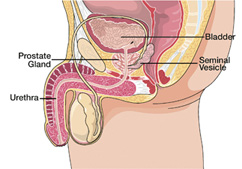 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of small cell prostate cancer. This particular form of prostate cancer is very rare. Small cell prostate cancer tends to occur in older men and is very aggressive. It is formed from hormone producing cells of the prostate, while standard prostate cancer is formed from glandular cells. Men with small cell prostate cancer often have an advanced stage of the disease when it is diagnosed. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Cancer occurs when cells in the prostate do not develop and die in their normal manner. The extra cells that result form a growth, or tumor, which can be benign or malignant. Benign tumors are not cancer and do not spread throughout the body. Malignant tumors are cancer. Their cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Men over the age of 45 are at the greatest risk for prostate cancer, which is the second most common cancer in men after skin cancer. A man’s chance of getting prostate cancer is increased when he has a family history of the condition, especially in his father or brother. However, no one truly knows why some men develop the condition and others do not. While the standard form of prostate cancer usually grows at a slow pace, small cell prostate cancer typically develops and metastasizes quickly. Your doctor may want to perform one or more tests to help determine if the cancer has spread, which could include the following: • MRI Scan Cancer that is located only within the prostate gland is the most manageable and curable. If malignant prostate cells are found beyond the prostate in the seminal vesicles, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable prostate cancer to help minimize pain and improve quality of life. |
Deciding on a treatment plan for your prostate cancer can be complex and depend upon a variety of factors, such as your age, general health condition, stage of cancer and personal preferences. The following treatment possibilities are available:
Hormone Therapy – Prostate cancer cells need male hormones, or androgens, such as testosterone to grow. Hormone therapy helps cancer shrink and grow more slowly by keeping the malignant cells from getting androgens. Methods used include drugs to block the production and effect of androgens and removal of the testicles, the main site of testosterone production. Because of its origin in hormone producing cells, small cell prostate cancer does not always respond well to hormone therapy.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread outside of the prostate and is unresponsive to hormone therapy.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a support group of other men with prostate cancer and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
National Cancer Institute, 800.422.6237, http://www.cancer.gov/
Us TOO International, 800.808.7866, http://www.ustoo.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Prostatic Intraepithelial Neoplasia
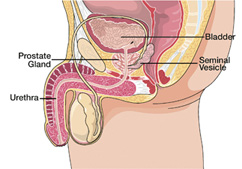 | After completing a thorough lab analysis of your recent prostate biopsy, a specialized doctor called a pathologist reported a diagnosis of prostatic intraepithelial neoplasia (PIN). This means that cells from your prostate gland showed abnormal development when compared to normal prostate cells. PIN is not cancer and may not produce any noticeable symptoms. As such, it generally does not require any treatment. Prostatic intraepithelial neoplasia is classified as either low-grade or high-grade. In low-grade PIN, abnormal cellular changes, or dysplasia, are slight and considered to be medically insignificant. Low-grade PIN is very common, with nearly half of all men having it by the age of 50. In high-grade PIN, dysplasia is moderate to severe, increasing the likelihood of developing prostate cancer. High-grade PIN may precede the development of cancer by five to 10 years in some men, and the incidence of the condition rises with age. Current literature has questioned whether patients with high-grade PIN are at greater risk for developing cancer over the men without high-grade PIN. |
Men with low-grade PIN have no greater risk of finding prostate cancer with repeat biopsies, so there is no need for additional testing other than annual prostate cancer screening checks. There is also no need for treatment.
For patients with high-grade PIN, repeat prostate biopsies are generally recommended. If no cancer is found in the repeat biopsies, men with high-grade PIN should continue to have cancer screenings (manual prostate checks and blood tests) and prostate biopsies on a regular basis.
Many doctors believe that high-grade PIN does not require any particular treatment other than monitoring. Others believe that treatment with certain drugs should be considered to possibly decrease the risk of cancer.
Because dietary factors have been associated with the development of prostate cancer, you should keep your diet high in fruits, vegetables and fiber and low in fat, especially animal fat. You may also want to boost your consumption of tomato products such as salsa, ketchup and tomato paste or sauce. They contain lycopene, a powerful antioxidant that helps prevent cell damage and the development of prostate cancer.
Soybeans and soy products are also good additions to your diet because they contain isoflavones, which act as antioxidants and may block the uncontrolled cell growth associated with cancer.
Further steps to help prevent prostate and other types of cancer include:
• Burning up all of the calories you take in each day through healthy eating and regular exercise
• Minimizing stress by getting enough sleep every night and using relaxation techniques
• Cutting out the use of tobacco and limiting your alcohol consumption
• Visiting your doctor regularly and promptly reporting any new symptoms that develop
American Cancer Society, 800.227.2345, http://www.cancer.org/
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 12.07
Prostatitis
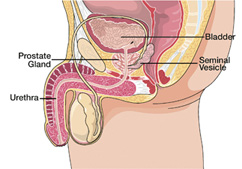 |
Your doctor has determined that you have prostatitis, an infection or inflammation of the prostate gland. The condition affects men of all ages, and is the most common urological disorder in those over age 50. About half of all men will experience prostatitis at some point. Prostatitis does not increase the risk of developing prostate cancer and it is not cancer. The prostate gland is typically the size of a walnut, located below the bladder and in front of the rectum in men. It surrounds a portion of the urethra, or tube that carries urine from the bladder out of the body. Its main purpose is to produce fluid for semen, which transports sperm. Prostatitis develops for a variety of reasons, and there are four main categories of the condition: • Nonbacterial Prostatitis Nonbacterial prostatitis and prostatodynia occur the most often. Bacterial prostatitis accounts for less than 10% of all cases. Nonbacterial prostatitis indicates an inflamed prostate without a bacterial infection. Prostatodynia, also called chronic pelvic pain syndrome, means that there are symptoms of prostatitis without inflammation or a bacterial infection. Possible sources of these forms of prostatitis include urinary reflux (urine flowing backward into the prostate ducts), physical injury, a nerve condition, muscle tension, urinary stones, a suppressed immune system and sexually transmitted diseases. Acute bacterial prostatitis happens most often in men under age 35, while the chronic variety mainly affects those ages 40 to 70. With acute bacterial prostatitis, severe complications can develop if it is not treated promptly. The infection can spread into the bloodstream and cause a life-threatening situation. With chronic bacterial prostatitis, the symptoms are less severe but recurring and are also likely to affect the urinary tract. Possible sources of bacterial prostatitis include a recent bladder infection or urinary catheterization and an abnormal urinary tract. |
Men with low-grade PIN have no greater risk of finding prostate cancer with repeat biopsies, so there is no need for additional testing other than annual prostate cancer screening checks. There is also no need for treatment.
For patients with high-grade PIN, repeat prostate biopsies are generally recommended. If no cancer is found in the repeat biopsies, men with high-grade PIN should continue to have cancer screenings (manual prostate checks and blood tests) and prostate biopsies on a regular basis.
Many doctors believe that high-grade PIN does not require any particular treatment other than monitoring. Others believe that treatment with certain drugs should be considered to possibly decrease the risk of cancer.
To help reduce the pain and inflammation of prostatitis and the need to strain when passing stools, which can aggravate prostate pain, you can:
• Take an over-the-counter medication such as ibuprofen or acetaminophen
• Employ hydrotherapy up to three times each day by sitting in a tub of hot water for 15–30 minutes
• Alternate cold soaks with hot soaks, or use hot and cold packs applied between the scrotum and anus (do not use heat if you have acute infection or inflammation)
• Avoid sugar, caffeine, dairy products, and fried and refined foods
• Drink plenty of water and eat healthy foods such as fruits and vegetables, whole grains, beans, soy, seeds and nuts, olive oil and cold-water fish (e.g., salmon, tuna, halibut, mackerel)
• Strive to minimize stress through exercise and relaxation techniques
• Take dietary supplements or herbs such as zinc, quercetin, vitamin E, saw palmetto, echinacea or goldenseal
Be sure to consult your doctor before taking any supplements or herbs.
American Foundation for Urologic Disease, 800.828.7866, http://www.afud.org/
The Prostatitis Foundation, 888. 891.4200, http://www.prostatitis.org/
Urology Channel, http://www.urologychannel.com/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07

