Acute Lymphoblastic Leukemia
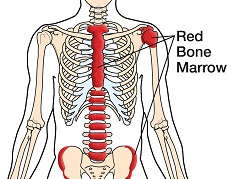 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of acute lymphoblastic leukemia (ALL), the most common type of leukemia in children but least common in adults, who account for about one-third of all cases. The soft inner tissue that fills the cavities of bones is called bone marrow. In adults, certain bones such as the skull, shoulder blades, ribs, pelvis and vertebrae (backbones) contain red bone marrow, which is the site of the body’s blood stem cells. These cells develop into blood-forming cells that then produce various components of the blood such as red and white blood cells and platelets. (Blood stem cells are not the same as embryonic stem cells.) Lymphocytes are a type of white blood cell made in the bone marrow that fight infection and include B- and T-cells and natural killer cells. Acute lymphoblastic leukemia is cancer that occurs when lymphocytes in the bone marrow do proliferate and mature in a normal manner. The extra cells that result can spread beyond the bone marrow to lymph nodes and organs such as the spleen or liver, which can become enlarged, as well as to the central nervous system (brain and spinal cord). The term acute refers to the fact that the disease is comprised of immature lymphocytes and progresses quickly without treatment. Symptoms of ALL may include fatigue, shortness of breath, weight loss, swollen lymph nodes, fever, excessive bruising or bleeding, upper abdominal discomfort and increased risk of infection. There are two main types of ALL, which reflect the type of lymphocytes where the cancer begins. B-cell ALL makes up about 85% of cases; T-cell ALL, about 15%. In very rare cases, the condition arises in the natural killer cells. There are several subtypes of the disease determined largely by the cancer’s genetics. Your doctor can tell you more about your particular subtype. |
Deciding on a treatment plan for ALL can be complex and depends upon a variety of factors such as your age, general health condition, ALL subtype, white blood cell count, other test results and personal preferences.
There are two phases of treatment for ALL — induction therapy and consolidation therapy. Induction therapy focuses on bringing about (inducing) a remission, which is the elimination of visible signs of the disease. Consolidation therapy, also known as post-remission therapy, seeks to destroy any remaining cancer cells and prevent a relapse.
The following treatment possibilities are available:
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, is the main treatment for ALL and provides a way to kill leukemia cells systemically (throughout the body) via the bloodstream, often through a combination of several drugs. Intrathecal chemotherapy is often used in the treatment of ALL, where it is injected directly into the cerebrospinal fluid of the central nervous system to kill leukemia cells that are not reached by standard forms of chemo. This helps prevent cancer from spreading to the brain or spinal cord, or treats it when it has already spread there.
Radiation Therapy – Radiation therapy is used to treat ALL that has spread to the brain and spinal cord, or to prevent its spread there. External beam radiation is generally used, in which a high energy X-ray machine directs radiation at the affected area(s).
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body along with healthy blood-forming cells in the bone marrow are destroyed by chemotherapy. Stem cells harvested from the bone marrow or blood of a matched donor are frozen and later thawed when needed for infusion into the body to help the bone marrow regenerate. When the stem cells come from a matched donor it is called an allogeneic transplant. When an ALL patient is in remission, an autologous transplant may be performed instead, which harvests stem cells from the patient rather than a donor.
Targeted Therapy – This newer form of anti-cancer therapy targets specific abnormalities within just the cancer cells to slow or stop their growth using drugs such as imatinib, dasatinib and nilotinib. It is used for certain ALL patients who may benefit from this type of treatment.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Keep all of your doctor’s appointments and promptly report any new symptoms or treatment side effects that develop. Also be sure to eat well including fruits and vegetables, get plenty of sleep and stay as active as you can.
American Cancer Society, 800.227.2345, www.cancer.org
The Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 8.12
Acute Myeloid Leukemia
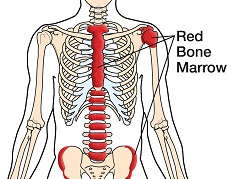 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of acute myeloid leukemia (AML), which is a type of blood cancer. The disease most often affects adults over the age of 65. The soft inner tissue that fills the cavities of bones is called bone marrow. In adults, certain bones such as the skull, shoulder blades, ribs, pelvis and vertebrae (backbones) contain red bone marrow, which is the site of the body’s blood stem cells. These cells develop into blood-forming cells that then produce various components of the blood such as red and white blood cells and platelets. (Blood stem cells are not the same as embryonic stem cells.) Acute myeloid leukemia is cancer that occurs when blood stem cells in the bone marrow do not proliferate, mature and expire in a normal manner. The extra cells that result can spread beyond the bone marrow to organs such as the spleen or liver, which can become enlarged. The term acute refers to the fact that the disease forms in immature bone marrow cells and progresses quickly without treatment. Symptoms of AML may include fatigue, fever, night sweats, increased risk of infection, weight loss, excessive bruising or bleeding, bone or joint pain, and anemia (reduced red blood cell count). Some patients experience skin rashes, swollen gums and abdominal swelling. There are multiple subtypes of the disease based on specific features of the cancer cells and their chromosomal structure (cytogenetics). Also an important distinction is made between AML cases that have an abrupt onset (de novo leukemia) and those that have a background of myelodysplasia, which are disorders in producing healthy mature blood cells. Your doctor can tell you more about your AML subtype. |
Although AML progresses rapidly, some subtypes respond well to treatment. Deciding on a treatment plan can be complex and depends upon a variety of factors, such as the disease subtype and your age, general health condition and personal preferences.
There are two phases of treatment for AML — induction therapy and consolidation therapy. Induction therapy focuses on bringing about (inducing) a remission, which is the elimination of visible signs of the disease. Consolidation therapy, also known as post-remission therapy, seeks to destroy any remaining cancer cells and prevent a relapse.
The following treatment possibilities are available:
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill leukemia cells systemically (throughout the body) via the bloodstream. Often a combination of several drugs is given, which varies based on the stage of cancer.
Other Drugs – Some patients who have the specific AML M3 subtype are treated with other drugs that may include all-trans retinoic acid or arsenic trioxide.
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body along with healthy blood-forming cells in the bone marrow are destroyed by the chemotherapy, which is given following the harvest of transplant cells from the bone marrow or blood of the patient (autologous transplant). This usual method has lower risks than allogeneic transplant, when cells come from a matched donor. The harvested cells are frozen and later thawed for infusion into the body to help the bone marrow regenerate.
Radiation Therapy – Radiation therapy is not generally used to treat AML, but it is employed in a few cases to reduce bone pain or treat cancer that has spread to the brain and spinal fluid or testicles. External beam radiation is generally used, in which a high energy X-ray machine directs radiation at the affected area(s).
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Keep all of your doctor’s appointments and promptly report any new symptoms or treatment side effects that develop. Also be sure to eat well including fruits and vegetables, get plenty of sleep and stay as active as you can.
American Cancer Society, 800.227.2345, www.cancer.org
The Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 8.12
Chronic Lymphocytic Leukemia
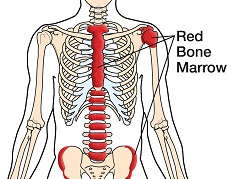 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of chronic lymphocytic leukemia (CLL), the most common form of leukemia in adults that affects mostly those over the age of 60. The soft inner tissue that fills the cavities of bones is called bone marrow. In adults, certain bones such as the skull, shoulder blades, ribs, pelvis and vertebrae (backbones) contain red bone marrow, which is the site of the body’s blood stem cells. These cells develop into blood-forming cells that then produce various components of the blood such as red and white blood cells and platelets. (Blood stem cells are not the same as embryonic stem cells.) Lymphocytes are a type of white blood cell made in the bone marrow that fight infection and includes B- and T-cells and natural killer cells. Chronic lymphocytic leukemia is cancer that occurs when lymphocytes in the bone marrow do not proliferate, mature and expire in a normal manner. The extra cells that result can spread beyond the bone marrow to lymph nodes and organs such as the spleen or liver, which can become enlarged. The term chronic refers to the fact that the disease forms in cells that appear mature, even though they are not truly normal. Many patients with CLL have no adverse effects; some may experience symptoms that include fatigue, fever, night sweats, swollen lymph nodes, upper abdominal discomfort, increased risk of infection and anemia (reduced red blood cell count). CLL can be slow- or fast-growing. There are five general stages of the disease — 0, I, II, III and IV — based on blood chemistry measurements and the extent of swelling in the lymph nodes, liver and spleen. Your doctor can tell you more about your cancer stage. |
Deciding on a treatment plan for CLL can be complex and depends upon a variety of factors such as your age, general health condition, stage of cancer and personal preferences. The following treatment possibilities are available:
Watchful Waiting – Some patients with slow-growing CLL decide not to pursue active therapy for their cancer but rather adopt a “watch and wait” tactic, avoiding the side effects of standard treatments.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill leukemia cells systemically (throughout the body) via the bloodstream. Often a combination of several drugs is given, which varies based on the stage of cancer.
Biologic Therapy – In certain cases, therapy that employs man-made biologics (i.e., synthetic proteins) such as rituximab and alemtuzumab is used to treat CLL. These biologics are called monoclonal antibodies and work by targeting specific proteins found on cancerous cells.
Radiation Therapy – Radiation therapy is not a main treatment for CLL, but does provide a way to reduce bone pain and discomfort caused by enlarged lymph nodes or organs. External beam radiation is generally used, in which a high energy X-ray machine directs radiation at the affected area(s).
Surgery – In rare cases when an enlarged spleen from CLL presses on other organs and causes pain, a splenectomy may be performed to remove it, which does not cure the leukemia but can improve blood cell counts.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also be sure to eat well including fruits and vegetables, get plenty of sleep and stay as active as you can.
American Cancer Society, 800.227.2345, www.cancer.org
The Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 8.12
Chronic Myeloid Leukemia
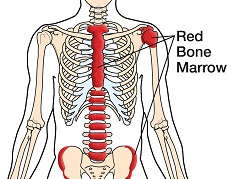 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of chronic myeloid leukemia (CML), which is a type of blood cancer that accounts for about 15% of leukemia cases. The average age at diagnosis is 65 and the disease most often affects adults. The soft inner tissue that fills the cavities of bones is called bone marrow. In adults, certain bones such as the skull, shoulder blades, ribs, pelvis and vertebrae (backbones) contain red bone marrow, which is the site of the body’s blood stem cells. These cells develop into blood-forming cells that then produce various components of the blood such as red and white blood cells and platelets. (Blood stem cells are not the same as embryonic stem cells.) Myeloid cells in the bone marrow are blood-forming cells that become mature red blood cells, platelets and certain types of white blood cells. Chronic myeloid leukemia is cancer that occurs when myeloid cells in the bone marrow do not proliferate, mature and expire in a normal manner. The extra cells that result can spread beyond the bone marrow to organs such as the spleen or liver, which may become enlarged. The term chronic refers to the fact that the disease is comprised of cells that appear mature, even though they are not truly normal. Many patients with CML have no adverse effects; some may experience symptoms that include fatigue, fever, night sweats, shortness of breath, increased risk of infection, weight loss, excessive bruising or bleeding, bone pain and upper left abdominal discomfort. There are three phases of the disease, based mainly on the percentage of myeloblasts (blasts), in the blood and bone marrow. These immature white blood cells gradually accumulate and block the production of healthy blood cells. About 85% of cases are Chronic CML, marked by less than 10% blasts and mild or no symptoms. Between 10–20% blasts are present along with other blood count factors and moderate symptoms in Accelerated CML. Blast Crisis CML is the most severe phase, with more than 20% blasts and more pronounced symptoms. Your doctor can tell you more about your CML phase. |
Deciding on a treatment plan for CML can be complex and depends upon a variety of factors, such as the phase of the disease and your age, level of spleen enlargement and personal preferences. The following treatment possibilities are available:
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill leukemia cells systemically (throughout the body) via the bloodstream. Often a combination of several drugs is given, which varies based on the stage of cancer.
Targeted Therapy – This newer form of anti-cancer therapy targets specific abnormalities within just the cancer cells to slow or stop their growth using drugs such as imatinib, dasatinib and nilotinib. It is used for certain CML patients who may benefit from this type of treatment.
Biologic Therapy – In certain cases, therapy that employs man-made biologics (i.e., synthetic proteins) such as interferon is used to treat CML.
Radiation Therapy – Radiation therapy is not a main treatment for CML, but does provide a way to reduce bone pain and discomfort caused by enlarged lymph nodes or organs. External beam radiation is generally used, in which a high energy X-ray machine directs radiation at the affected area(s).
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body along with healthy blood-forming cells in the bone marrow are destroyed by chemotherapy. Stem cells harvested from the bone marrow or blood of a matched donor are frozen and later thawed when needed for infusion into the body to help the bone marrow regenerate. When the stem cells come from a matched donor it is called an allogeneic transplant. Allogeneic stem cell transplant is the only treatment that may cure some CML patients, but not all patients are candidates for the procedure.
Donor Lymphocyte Infusion – After stem cell transplant, certain CML patients may also receive an infusion of lymphocytes from their stem cell donor. The transferred lymphocytes — a type of white blood cell made in the bone marrow that fights infection — can trigger an immune reaction in the patient against any remaining cancer cells.
Leukapheresis – Some CML patients may have excess white blood cells removed from their blood via leukapheresis, which is a process similar to dialysis.
Surgery – In rare cases when an enlarged spleen from CML presses on other organs and causes pain, a splenectomy may be performed to remove it, which does not cure the leukemia but can improve blood cell counts.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Keep all of your doctor’s appointments and promptly report any new symptoms or treatment side effects that develop. Also be sure to eat healthy foods and stay as active as you can.
American Cancer Society, 800.227.2345, www.cancer.org
The Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 8.12
Hodgkin Lymphoma
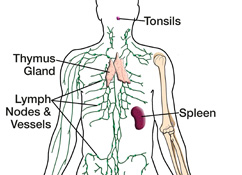 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of Hodgkin lymphoma, which is a type of cancer that develops in certain lymphatic system cells called lymphocytes. Cases are most often diagnosed in patients between the ages of 15–40 and over the age of 55. Previously referred to as Hodgkin’s disease, Hodgkin lymphoma is one of the most curable forms of cancer, with about 80% of patients attaining a full recovery. The lymphatic system is comprised of lymph nodes, vessels and fluid, as well as related organs. Part of the immune system, it helps the body fight infections, delivers oxygen, nutrients and hormones to the cells, and filters harmful substances such as bacteria and waste from the lymph fluid. More than 600 bean-shaped lymph node glands are connected by a vast network of lymphatic vessels that transport the colorless lymph fluid, which originates in the blood as plasma and returns to the bloodstream after traveling through the lymph system. The lymph nodes and organs such as the tonsils, thymus and spleen are made of lymphoid tissue that contains a large amount of lymphocytes (such as B- and T-cells), a type of white blood cell that fights infection. Lymphoma is a type of cancer that occurs when lymphocytes in lymph nodes or lymphatic organs do not develop and die in their normal manner. The extra cells that result can form a growth, or tumor, and spread to adjacent lymph nodes, invade and damage other nearby lymph nodes or organs, or spread further to other locations in the body. There are two types of Hodgkin lymphoma based on specific features of the cancer cells. Nodular sclerosis, mixed cellularity, lymphocyte-rich and lymphocyte-depleted subtypes fall under the category of classical Hodgkin lymphoma and account for about 95% of cases. Lymphocyte predominant Hodgkin lymphoma is comprised of the subtypes diffuse lymphocyte predominant (very rare) and nodular lymphoctye predominant, which makes up nearly 5% of cases. There are four general stages of Hodgkin lymphoma (I, II, III, IV) based on whether and how much the cancer has spread. In addition, each stage can be characterized with a “B” to denote if certain symptoms (such as weight loss, night sweats and fever) are present or an “A” to denote the absence of such B symptoms. Your doctor can tell you more about your particular cancer subtype and stage. |
Deciding on a treatment plan for Hodgkin lymphoma can be complex and depend upon a variety of factors such as the disease subtype and stage, and your age, general health condition and personal preferences. Chemotherapy and radiation therapy are the two main treatments used, either separately or together (combined modality therapy), depending on case specifics. The following treatment possibilities are available:
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill lymphoma cells systemically (throughout the body) via the bloodstream. A combination of several drugs is given, which varies based on the stage of cancer.
Radiation Therapy – Radiation therapy provides a way to shrink or destroy masses of cancer cells as well as to reduce pain. For Hodgkin lymphoma, external beam radiation is used, in which a high energy X-ray machine directs radiation at the affected lymph nodes or other areas.
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body and healthy blood-forming cells in the bone marrow are destroyed by the chemotherapy, which is given following the harvest of transplant cells from the bone marrow or blood of the patient (autologous transplant). This usual method has lower risks than allogeneic transplant, when cells come from a matched donor. The harvested cells are frozen and later thawed for infusion into the body to help grow new bone marrow. Stem cell transplant is used for patients whose cancer has come back (recurred) or not fully responded to previous treatments.
Biologic Therapy – In certain cases, therapy that employs man-made biologics (i.e., synthetic proteins) such as brentuximab vedotin or rituximab is used to treat Hodgkin lymphoma. These biologics are called monoclonal antibodies and work by targeting specific proteins found on cancerous cells.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep every night, keep all of your doctor’s appointments and promptly report any new symptoms or treatment side effects that develop.
American Cancer Society, 800.227.2345, www.cancer.org
Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
Lymphoma Research Foundation, 800.500.9976, www.lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 1.12
Multiple Myeloma
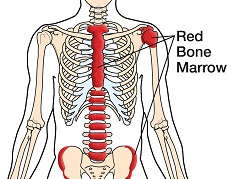 | After completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of multiple myeloma, which is a type of cancer that develops from plasma cells. The average age the condition begins is in the mid-60s, and men are affected more often than women. The soft inner tissue that fills the cavities of bones is called bone marrow. In adults, certain bones such as the skull, shoulder blades, ribs, pelvis and vertebrae (backbones) contain red bone marrow, which is the site of the body’s blood stem cells. These cells develop into blood-forming cells that then produce various components of the blood such as red and white blood cells and platelets. (Blood stem cells are not the same as embryonic stem cells.) Plasma cells are a type of white blood cell that make proteins called antibodies, which are part of the immune system that helps protect the body from harmful substances such as bacteria. Myeloma is a type of cancer that occurs when plasma cells do not develop and die in a normal manner. The abnormal cells collect in the bone marrow and may damage the solid part of a bone, causing bone pain and fractures. Multiple myeloma is when more than one bone is affected, and plasmacytoma is the name when there is only one focus of disease. The extra abnormal proteins made by myeloma cells can cause complications such as an increased risk of infections due to reduced immunity, impaired kidney function, headaches, and impaired vision. Sometimes they may form deposits that cause organ damage, called amyloidosis. There are three general stages of multiple myeloma — I, II and III — based on blood chemistry measurements and how much the bones and other organs have been affected by the cancer. Your doctor can tell you more about your particular cancer subtype and stage. |
Deciding on a treatment plan for multiple myeloma can be complex and depends upon a variety of factors such as your age, general health condition, stage of cancer and personal preferences. The following treatment possibilities are available:
Watchful Waiting – Some patients with early or Stage I multiple myeloma decide not to pursue active therapy for their cancer but rather adopt a “watch and wait” tactic, avoiding the side effects of standard treatments.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill myeloma cells systemically (throughout the body) via the bloodstream. Often a combination of several drugs is given, which varies based on the stage of cancer.
Targeted Therapy – This newer form of anti-cancer therapy targets specific abnormalities within just the cancer cells to slow or stop their growth using drugs such as bortezomib.
Biologic Therapy – In certain cases, therapy that employs man-made biologics (i.e., synthetic proteins) such as interferon is used to treat multiple myeloma.
Other Drugs – Bisphosphonates are drugs that can help slow down the bone weakening process in multiple myeloma patients. Thalidomide and lenalidomide are often used due to various beneficial effects that fight the cancer. Corticosteroids are also used at times to treat multiple myeloma.
Radiation Therapy – Radiation therapy provides a way to shrink or destroy masses of cancer cells as well as to reduce pain. For multiple myeloma, external beam radiation is used, in which a high energy X-ray machine directs radiation at the tumor.
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body along with healthy blood-forming cells in the bone marrow are destroyed by the chemotherapy, which is given following the harvest of transplant cells from the bone marrow or blood of the patient (autologous transplant). This usual method has lower risks than allogeneic transplant, when cells come from a matched donor. The harvested cells are frozen and later thawed for infusion into the body to help the bone marrow regenerate.
Plasmapheresis – Some patients who experience a buildup of myeloma proteins and thickening of the blood (hyperviscosity) receive plasmapheresis, which may help with symptoms but does not kill cancer cells. The process involves removing blood from the body via a vein, separating the plasma from the blood cells, discarding the plasma (which contains abnormal protein) and returning the blood to the patient, with the plasma replaced by a salt solution or donor plasma.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also be sure to eat well, including protein to keep up your strength, drink plenty of fluids and stay as active as you can.
American Cancer Society, 800.227.2345, www.cancer.org
Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 8.12
Myelodysplastic Syndromes
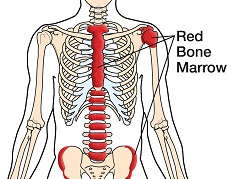 | The soft inner tissue that fills the cavities of bones is called bone marrow. In adults, certain bones such as the skull, shoulder blades, ribs, pelvis and vertebrae (backbones) contain red bone marrow, which is the site of the body’s blood stem cells. These cells develop into blood-forming cells that then produce various components of the blood such as red and white blood cells and platelets. (Blood stem cells are not the same as embryonic stem cells.) Myelodysplastic syndromes (MDS) are cancers that occur when myeloid cells in the bone marrow do not proliferate and mature effectively, leading to low blood counts, and the cells that do get released into the blood are somewhat defective. The cause of the disease is often not known, in which case it is classified as primary MDS. When it occurs as a response to chemotherapy or exposure to radiation, heavy metals or certain chemicals, it is called secondary MDS, which includes treatment-related MDS. Symptoms may include fatigue, shortness of breath, increased risk of infection, excessive bruising or bleeding, and anemia (reduced red blood cell count). A small percentage of MDS patients develop acute myeloid leukemia, but most do not. MDS is classified into several types, such as refractory anemia, based on specific features of the bone marrow, blood cell counts and other factors. The stage of the disease is reflected by the International Prognostic Scoring System (IPSS), which assigns risk levels into four groups: low, intermediate-1, intermediate-2, and high. Your doctor can tell you more about your particular type of MDS and risk level. |
Different types of MDS vary in how well they respond to treatment; some treatment options focus primarily on relieving symptoms and improving quality of life. Deciding on a treatment plan for MDS can be complex and depends upon a variety of factors, such as the disease risk level and type, and your age, general health condition and personal preferences. The following treatment possibilities are available:
Watchful Waiting – Some low-risk or intermediate-1 MDS patients decide not to pursue active therapy but adopt a “watch and wait” tactic, avoiding the side effects of standard treatments.
Transfusion Therapy – Some MDS patients are given red blood cells or platelets via blood transfusions to improve their blood counts. This form of treatment can help relieve fatigue and shortness of breath.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill cancer cells systemically (throughout the body) via the bloodstream. Often a combination of several drugs is given, which varies based on the stage of cancer.
Hypomethylating Agents (Epigenetic Therapy) – Another form of chemotherapy involves the use of hypomethylating agents, which reactivate switched-off tumor-suppressor genes that usually protect cells from becoming cancerous. Azacitidine and decitabine are two such drugs used to treat low- and high-risk MDS patients, and can help reduce the need for blood transfusions.
Growth Factors – Erythropoietin (EPO) is a hormone made in the kidneys that assists the body in producing blood cells. A small percentage of MDS patients who have low levels of EPO are given growth factors called erythropoietin-stimulating agents to promote red blood cell production and help reduce the need for blood transfusions. At times another hormone to stimulate white blood cell production may be given.
Immunotherapy – Antithymocyte globulin is an immunosuppressing drug that destroys abnormal T-lymphocytes, which are a type of white blood cell that can interfere with normal blood cell production in patients with certain MDS subtypes. Immunomodulating agents such as lenalidomide are sometimes used to stimulate the immune system and lessen the need for red blood cell transfusions for certain MDS patients who may benefit from the therapy.
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body along with healthy blood-forming cells in the bone marrow are destroyed by chemotherapy. Stem cells harvested from the bone marrow or blood of a matched donor are frozen and later thawed when needed for infusion into the body to help the bone marrow regenerate. When the stem cells come from a matched donor it is called an allogeneic transplant. Allogeneic stem cell transplant is the only treatment that may cure some MDS patients, but not all patients are candidates for the procedure.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Keep all of your doctor’s appointments and promptly report any new symptoms or treatment side effects that develop. Also be sure to eat a healthy diet and stay as active as you can.
American Cancer Society, 800.227.2345, www.cancer.org
Myelodysplastic Syndromes Foundation, 800.637.0839, www.mds-foundation.org
The Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 8.12
Non-Hodgkin Lymphoma
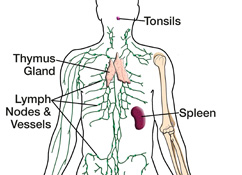 |
fter completing a thorough lab analysis of your recent biopsy, a specialized doctor called a pathologist reported a diagnosis of non-Hodgkin lymphoma (NHL), which is a type of cancer that develops in certain lymphatic system cells called lymphocytes. The average age at the time of diagnosis is 60; about half of all cases occur in patients age 65 and older. The lymphatic system is comprised of lymph nodes, vessels and fluid, as well as related organs. Part of the immune system, it helps the body fight infections, delivers oxygen, nutrients and hormones to the cells, and filters harmful substances such as bacteria and waste from the lymph fluid. More than 600 bean-shaped lymph node glands are connected by a vast network of lymphatic vessels that transport the colorless lymph fluid, which originates in the blood as plasma and returns to the bloodstream after traveling through the lymph system. The lymph nodes and organs such as the tonsils, thymus and spleen are made of lymphoid tissue that contains a large amount of lymphocytes, a type of white blood cell that fights infection and includes B- and T-cells and natural killer cells. Lymphoma is a type of cancer that occurs when lymphocytes in lymph nodes or lymphatic organs do not develop and die in their normal manner. The extra cells that result can form a growth, or tumor, and spread to adjacent lymph nodes, invade and damage other nearby lymph nodes or organs, or spread further to other locations in the body. Non-Hodgkin lymphoma is classified by the pace of the disease and the subtype, which is based on specific features of the cancer cells. Indolent (low-grade) NHL grows slowly while aggressive (high-grade) NHL grows more rapidly. B-cell NHL subtypes are the most common — up to 85–90% of cases — and include mucosa-associated lymphatic tissue (MALT) lymphoma and diffuse large B-cell lymphoma, the most common NHL accounting for nearly a third of all cases. T-cell and natural killer cell subtypes account for 10–15% of cases and include peripheral T-cell lymphoma and anaplastic large cell lymphoma. There are four general stages of non-Hodgkin lymphoma (I, II, III, IV) based on whether and how much the cancer has spread. In addition, each stage can be characterized with a “B” to denote if certain symptoms (such as weight loss, night sweats and fever) are present or an “A” to denote the absence of such B symptoms. Your doctor can tell you more about your particular cancer subtype and stage. |
Deciding on a treatment plan for non-Hodgkin lymphoma can be complex and depend upon a variety of factors such as the disease pace, subtype and stage, and your age, general health condition and personal preferences. The following treatment possibilities are available:
Watchful Waiting – Some patients with indolent NHL decide not to pursue active therapy for their cancer but rather adopt a “watch and wait” tactic, avoiding the side effects of standard treatments.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to kill lymphoma cells systemically (throughout the body) via the bloodstream. Often a combination of several drugs is given, which varies based on the stage of cancer.
Radiation Therapy – Radiation therapy provides a way to shrink or destroy masses of cancer cells as well as to reduce pain. For non-Hodgkin lymphoma, external beam radiation is used, in which a high energy X-ray machine directs radiation at the affected lymph nodes or other areas.
(Hematopoietic) Stem Cell Transplant – Stem cell transplant involves the transfer of specific blood-forming (hematopoietic) cells after high-dose chemotherapy (and at times added radiation therapy). Cancer cells in the body and healthy blood-forming cells in the bone marrow are destroyed by the chemotherapy, which is given following the harvest of transplant cells from the bone marrow or blood of the patient (autologous transplant). This usual method has lower risks than allogeneic transplant, when cells come from a matched donor. The harvested cells are frozen and later thawed for infusion into the body to help grow new bone marrow. Stem cell transplant is used for patients whose cancer has come back (recurred) or not fully responded to previous treatments.
Biologic Therapy – In certain cases, therapy that employs man-made biologics (i.e., synthetic proteins) such as rituximab or alemtuzumab is used to treat non-Hodgkin lymphoma. These biologics are called monoclonal antibodies and work by targeting specific proteins found on cancerous cells.
Targeted Therapy – This newer form of anti-cancer therapy targets specific abnormalities within just the cancer cells to slow or stop their growth using drugs such as bortezomib and temsirolimus.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group, and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep every night, keep all of your doctor’s appointments and promptly report any new symptoms or treatment side effects that develop.
American Cancer Society, 800.227.2345, www.cancer.org
Leukemia & Lymphoma Society, 800.955.4572, www.leukemia-lymphoma.org
Lymphoma Research Foundation, 800.500.9976, www.lymphoma.org
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 1.12

