Actinic Keratoses
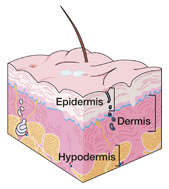 | Your doctor has determined that you have actinic keratoses, or scaly, rough-textured patches on the surface of your skin. Actinic keratoses (AKs) are not cancer but are the most common type of precancerous skin lesion, affecting more than 10 million Americans. The skin is the largest organ of the body. Its top layer is the epidermis, which contains three types of cells that can become cancerous: melanocytes, basal cells and squamous cells. The main purpose of the epidermis is to provide protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Actinic keratoses — also called solar keratoses — occur when the squamous cells of the epidermis are damaged from longterm ultraviolet (UV) light exposure, usually from the sun. Because skin damage accumulates over a lifetime, even brief amounts of time in the sun contribute to a person's total exposure. Most AKs are found on the face, ears, scalp, neck, forearms, back of the hands and shoulders. The most aggressive form occurs on the lips and is called actinic cheilitis. AKs usually develop slowly and vary in size from a pinhead to larger than a quarter. They can be flat or raised with a tan, pink, reddish-brown or skin-tone appearance. The lesions have a dry, crusty feeling and may occasionally grow into a horn shape, called a cutaneous horn. Usually they are not bothersome, but at times they can itch, cause tenderness or become inflamed. People age 40 and older with fair skin, blonde or red hair and blue, green or gray eyes are at an increased risk for actinic keratoses. However, younger people and those with darker skin and eyes can also develop AKs from too much sun exposure. Other risk factors include: • Living in sunny locations or regions near the equator Most actinic keratoses can be eliminated if they are treated early. If left untreated, AKs can progress to a type of skin cancer called squamous cell carcinoma over a period of time. Although squamous cell carcinoma is the second leading cause of skin cancer deaths in the U.S., the condition is usually not life-threatening if found and treated early. People with actinic keratoses are also at a higher risk for developing other types of skin cancer due to their accumulated sun damage. |
The usual treatment for actinic keratoses is removal by a doctor, which may be accomplished in one of several ways depending on factors such as lesion size and location and your age, general health condition and personal preferences. Sometimes more than one treatment may be used at the same time. The following treatment possibilities are available:
Cryosurgery – The most common treatment method for AKs is cryosurgery, which uses super-cooled gas to freeze and destroy lesions.
Topical Medication – Another common treatment is the application of medicated cream directly onto the skin (topically) to destroy lesions, most often the drug 5-fluorouracil.
Excision – Cutting or shaving off lesions with a scalpel (excision) is also a common treatment.
Curettage and Electrocautery – This common procedure uses a curette (sharp scooping instrument) to remove AKs, then an electrified needle to stop the bleeding.
Laser Therapy – Sometimes a high-intensity light, or laser, is used to burn off actinic keratoses.
Photodynamic Therapy – Lesions can be also be burned off by a laser light after being illuminated by a photosensitizing drug.
Chemical Peeling – This method destroys AKs by using a chemical agent applied to the skin.
Dermabrasion – AKs can also be removed by "sanding" them off, known as dermabrasion.
Retinoids – Occasionally a retinoid cream, which is derived from vitamin A, is prescribed for topical use to help prevent new lesions from developing.
Steps you can take to prevent further actinic keratoses and skin cancer include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing long sleeves and pants, a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
• Visiting your doctor regularly for skin checks and promptly reporting any new lesions that develop
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
American Cancer Society, 800.227.2345, http://www.cancer.org/
Skin Cancer Foundation, 800.754.6490, http://www.skincancer.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 10.07
Basal Cell Carcinoma
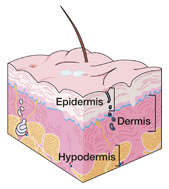 | After completing a thorough lab analysis of your skin biopsy under a microscope, a specialized doctor called a pathologist reported a diagnosis of basal cell carcinoma, which is the most common form of skin cancer and, in fact, the most common of all types of cancer. Nearly 90% of all skin cancers are basal cell carcinomas, and the condition affects about 800,000 Americans each year.The skin is the largest organ of the body. Its top layer is the epidermis, which contains three types of cells that can become cancerous: melanocytes, basal cells and squamous cells. The main purpose of the epidermis is to provide protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis.Basal cell carcinoma occurs when basal cells in the epidermis do not develop and die in their normal manner because of damage from long-term ultraviolet (UV) light exposure, usually from the sun. The extra cells that result form a cancerous (malignant) growth, or tumor. Most basal cell tumors are found on the head, neck, shoulders, chest, arms, back or legs. People age 40 and older with fair skin, blonde or red hair and blue, green or gray eyes are at a higher risk for the condition, as are those who work or spend much time outdoors. The appearance of basal cell carcinoma may vary. Often it looks like a pearly or transparent white, pink or red bump. In darker haired people, the bump may be tan, black or brown. A basal cell tumor can also look like: • An open sore that bleeds, oozes or crusts Basal cell carcinoma grows slowly and generally does not spread to other parts of the body but can grow into surrounding tissue, so it is important to find and treat it early. People with the condition have about a 40% chance of developing another basal cell tumor within five years. They are also at a higher risk for developing other types of skin cancer due to their accumulated sun damage. |
The usual treatment for basal cell carcinoma is removal by a doctor, which may be accomplished in one of several ways depending on factors such as tumor size and location and your age, general health condition and personal preferences. In some cases with certain treatment methods, reconstructive surgery using a skin flap or graft may be required. The following treatment possibilities are available for basal cell carcinoma:
Cryosurgery – This treatment uses super-cooled gas to freeze and destroy basal cell tumors.
Excision – Cutting out tumors with a scalpel (excision) is a traditional treatment for the condition.
Curettage and Electrocautery – This most common treatment method uses a curette (sharp scooping instrument) to remove tumors, then an electrified needle to stop the bleeding.
Laser Therapy – Sometimes a high-intensity light, or laser, is used to destroy basal cell carcinoma.
Photodynamic Therapy – Tumors can also be burned off by a laser light after being illuminated by a photosensitizing drug.
Radiation Therapy – Another treatment method is radiation therapy, which uses a high energy X-ray machine to direct radiation at the tumor. It is often favored for cancers in areas that are difficult to treat and for recurrent lesions that were previously treated surgically.
Mohs Micrographic Surgery – Performed by a dermatologic surgeon, this highly specialized procedure has the highest cure rate of all basal cell carcinoma treatments and provides a minimal amount of tissue removal. During Mohs surgery, a tumor is removed in microscopic sections, one layer at a time. The surgeon examines each section under a microscope to determine if all of the cancer is gone, or if additional layers need to be removed.
Topical Immunotherapy – This form of treatment for surface tumors involves the application of a medicated cream (imiquimod) directly onto the skin, or topically, to stimulate the body's immune responses to fight the cancer.
After treatment, your doctor will likely recommend that you have periodic skin cancer screening exams to monitor your condition.
Steps you can take to prevent further skin damage and occurrences of skin cancer include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing long sleeves, pants, a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
American Cancer Society, 800.227.2345, http://www.cancer.org/
Skin Cancer Foundation, 800.754.6490, http://www.skincancer.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 10.07
Common Warts
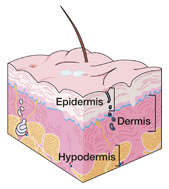 |
Your doctor has determined that you have one or more common warts, which are small skin growths caused by a virus. They are not cancer and do not increase the risk of developing skin cancer. Warts can occur at any time of life, although they often appear between the ages of 12 and 16. They are the second most common skin complaint, just after acne. The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis.Common warts — also called verrucae vulgaris — occur when areas in the surface layer of the skin grow faster than normal due to infection with one of the many types of wart-causing human papilloma virus (HPV). The resulting benign, or harmless, growths are usually bumpy and gray, white, pink or flesh-toned, but can also be dark and smooth. They often contain small black dots that look like seeds, which are clotted blood vessels within the warts.The hands are the usual site of common warts, especially around the fingernails. Warts can spread to other parts of the body and to other people through direct or indirect contact. Some people are more prone to getting wart-causing HPV than others, and the virus occurs more easily in places where the skin has been injured.In addition to common warts, two other main types of warts affect non-genital areas of the body: flat warts and foot, or plantar, warts. Flat warts, or verrucae plana, are much smaller and smoother than other warts and grow in groups of 20 to 100. They occur most often on the face in men and the legs in women. Plantar warts, or verrucae plantaris, can occur singly or in a cluster and are usually found on the soles of feet. They grow inwardly rather than protruding from the skin because of the pressure from walking. Plantar warts can be painful and feel like a stone in the shoe. |
Deciding on a treatment plan for your warts can depend upon a variety of factors such as their type and location and your age. Sometimes warts are left untreated because they may go away on their own. Up to 30% of warts spontaneously disappear within six months; the majority disappear within three years. Many times, however, warts are removed by a doctor to prevent spreading, deal with bothersome symptoms and improve the appearance of the skin. This may be accomplished in one of several ways:
Cryosurgery – This most common method of treatment uses super-cooled gas to freeze and destroy warts. Stubborn warts may require repeat treatments.
Topical Medication – Another common treatment is the application of medication directly onto the skin (topically) to destroy warts. The drug cantharidin is often used for this type of therapy. Other medications that may be used include retinoids, podofilox, tretinoin and podophyllum.
Curettage – This procedure uses a curette (sharp scooping instrument) to scrape off warts.
Electrocautery – In electrocautery, an electrified needle is used to destroy warts.
Laser Therapy – Sometimes a high-intensity light, or laser, is used to treat certain types of warts.
Interferon Therapy – Another treatment choice is the injection of interferon directly into the warts.
Other Therapies – A variety of other therapies may be used to treat warts such as the injection of the drug bleomycin and biologic therapy with topical imiquimod cream, which enhances the immune system's ability to reject the warts.
In some cases, surgery to cut out warts may be necessary if other treatment methods do not prove to be successful.
To make sure that you do not spread warts to other parts of your body or to other people and to minimize your chance of developing new warts, you should take the following steps:
• Avoid touching or picking at warts on yourself or others
• Wash your hands thoroughly if they do come in contact with warts
• Keep your warts covered if possible
• Avoid biting your nails or picking at hangnails
• Keep your hands away from your face
• Avoid going barefoot in public places
• Keep your feet clean and dry
• Change your shoes and socks each day
• Wear water shoes while in locker rooms, swimming pools and saunas
• Avoid sharing towels, combs, brushes or footwear with anyone
• Treat new warts as quickly as they develop
Eating healthy meals high in vitamins A, C and E and minimizing stress can help boost your immune system against HPV. Also, be sure to promptly report any changes in your skin to your doctor.
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Contact Dermatitis
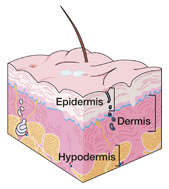 | The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Contact dermatitis occurs when the skin reacts to direct contact with a triggering substance. There are two main types of contact dermatitis: allergic and irritant. Allergic contact dermatitis indicates an overreaction of the body's immune system to a normally harmless substance. Common causes of allergic contact dermatitis include: • Plants such as poison ivy, poison oak, ragweed and primrose Irritant contact dermatitis, which occurs when the skin comes in contact with an irritating, harsh or dangerous substance, accounts for about 80% of contact dermatitis cases. The longer the substance stays on the skin, the more severe the reaction becomes. Common causes of irritant contact dermatitis include industrial cleaning products, solvents, drain cleaners, turpentine, dishwashing and other detergents, soaps and household cleaners. Sometimes contact dermatitis happens after a person touches a substance then exposes that area of skin to sunlight, which is called photoallergic contact dermatitis. Contact with the substance by itself and sun exposure without the presence of the substance do not cause a reaction. It only occurs as a combination of the two factors. Common causes of photoallergic contact dermatitis include sunscreens, cosmetics, aftershaves and perfumes, antibiotics, coal tar and oils. |
Contact dermatitis can be treated in a variety of ways, but treatment is generally not effective until there is no further contact with the triggering substance. Then it may take up to four weeks for the irritated area to return to normal. The following treatment possibilities are available:
Soothing Therapies – Cool cloth or gauze compresses soaked in water or aluminum acetate (Burow's solution) can be applied for up to an hour several times a day to help ease the symptoms of contact dermatitis. Other soothing therapy choices include calamine lotion (not containing diphenhydramine) and cool tub baths with added bath oil or colloidal oatmeal.
Oral Antihistamines – Over-the-counter (OTC) or prescription oral antihistamines may be recommended to help relieve itching. Antihistamine creams, however, are not recommended for treating contact dermatitis.
Corticosteroids – An OTC hydrocortisone or prescription-strength corticosteroid cream may be used to treat contact dermatitis. For severe cases, an oral corticosteroid pill or corticosteroid injection may be prescribed.
Antibiotics – When an infection develops at the site of contact dermatitis, antibiotics may be prescribed to treat the infection.
In addition, the liberal use of emollient moisturizers is recommended to protect the skin as it recovers from a bout of contact dermatitis.
Steps you can take to further reduce symptoms and prevent future occurrences of contact dermatitis include:
• Avoiding scratching if you have a skin reaction
• Finishing your recommended treatment program and all prescription medications
• Avoiding all substances that trigger your contact dermatitis
• Washing the skin immediately with soap and cool water if exposed to a triggering substance
• Using sunscreens that do not contain PABA
• Wearing gloves and long sleeves and pants if you are working outdoors
• Using fragrance-free products when possible
• Covering objects containing nickel with clear nail polish or a special spray and wearing earrings that have surgical steel posts
• Using a barrier cream to block the action of certain substances, such as poison ivy
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
Asthma and Allergy Foundation of America, 202.466.7643, http://www.aafa.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Cutaneous Neurofibromas
|
| Your doctor has determined that you have one or more cutaneous neurofibromas, which are benign skin growths that arise from nerve connective tissue. They are not cancer and do not normally increase the risk of developing skin cancer. Cutaneous neurofibromas can occur at any time of life, although they often appear between the ages of 20 and 30. he skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Cutaneous neurofibromas occur when cells in the covering of a nerve (the nerve sheath) in the skin form a slow-growing, soft and usually painless growth, or tumor. These normally benign, or harmless, tumors can vary in size, are flesh-toned and have broad or stalk-like bases. Cafe au lait spots, which look similar to the color of coffee with milk and can range in size from small to very large, are another type of cutaneous neurofibroma. They typically develop on the chest, back, pelvis, elbows and knees, although they can appear on many other parts of the body. In addition to cutaneous neurofibromas, there are three other main types of neurofibromas, which can occur anywhere in the body except the brain and spinal cord: • Subcutaneous neurofibromas, which lie deeper under the skin and can sometimes be tender |
The usual treatment for cutaneous neurofibromas is removal by a doctor, which may be accomplished in one of a few ways. In some cases, reconstructive surgery using a skin flap or graft may be required. The following treatment possibilities are available:
Excision – Cutting out cutaneous neurofibromas with a scalpel (excision) is the most often used method of removal. In some cases it may also be necessary to remove the nerve.
Radiation Therapy – Radiation therapy can reduce cutaneous neurofibromas by using a high energy X-ray machine to direct radiation at the tumors.
Cutaneous neurofibromas rarely come back after they are removed. If you have any new growths or related abnormal sensations such as tingling, promptly report them to your doctor.
To maximize your health and minimize your risk of ever developing skin cancer, you should strive to prevent skin damage from ultraviolet (UV) ray exposure. General steps you can take include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
• Visiting your doctor regularly for skin cancer screenings
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Discoid Lupus Erythematosus
|
| Your doctor has determined that you have discoid lupus erythematosus (DLE), a chronic, or ongoing, condition that causes coin-shaped skin lesions. DLE occurs more than twice as often in women as men and can happen at any age, but it most often appears in people age 20 to 40. The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Discoid lupus erythematosus causes lesions on the skin that are round, red and scaly. Over time they can thicken, extend outward or merge with other lesions and cause scarring and discoloration. When lesions affect the scalp, they often plug hair follicles and lead to hair loss, which can be permanent. Most people with DLE have no noticeable symptoms other than the appearance of lesions, though some may experience mild itching. Sun exposure usually aggravates the condition. There are two main forms of DLE: localized and generalized. Localized lesions are limited to the head and neck, while generalized lesions affect other parts of the body as well. Most DLE lesions appear on sun-exposed areas of the skin and may stay or recur for years. Other varieties of DLE can sometimes occur, such as wart-like lesions, lesions on the hands and feet, lesions accompanied by lumps in the underlying fatty tissue or lesions in the mucus membranes of the mouth, nose and eyes. Discoid lupus erythematosus is thought to have a genetic component, but its exact cause is unknown. The condition appears to stem from an overactive immune system response, usually after ultraviolet (UV) light exposure from the sun. Other contributing factors likely play a role in its development. DLE is related to the disease systemic lupus erythematosus (SLE), in which the body's immune system attacks and damages various tissues and organs. SLE can be very mild to extremely serious, sometimes with life-threatening complications. About 10% of patients with DLE develop SLE, but usually not at a severe level. |
Enter body of accordion
The typical treatment plan for discoid lupus erythematosus seeks to improve the appearance of the skin, limit scarring, control current lesions and prevent future outbreaks. The following treatment possibilities are available:
Corticosteroids – One treatment method for DLE is the application of corticosteroids directly onto the skin (topically) via a cream, ointment, foam or medicated tape. In some cases, corticosteroid injections are given directly into the lesions.
Antimalarials – DLE lesions that are widespread or do not respond to corticosteroids can be treated with oral antimalarials, or drugs that are primarily used to treat the infectious disease malaria.
Other Medications – In addition to corticosteroids and antimalarials, other medications are sometimes prescribed to treat DLE. They include topical retinoids, which are derived from vitamin A, and stronger drugs that suppress the immune system.
After treatment, your doctor will likely recommend that you have follow-up exams at regular intervals to monitor your condition.
You can protect your skin and help prevent further DLE outbreaks by minimizing your exposure to UV light. Specific steps you can take to reduce flare-ups include:
• Avoiding the sun — especially between 10 a.m. and 4 p.m. when UV rays are the strongest —as well as sunlight reflected by sand, water or snow
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing tightly-woven or special sun-protective clothing, long sleeves and pants, a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices, as well as unshielded fluorescent light tubes
• Stopping smoking, which can aggravate the condition and interfere with the effectiveness of some medications
• Eating a healthy diet low in red meat and dairy products and high in cold-water fish (e.g., salmon, tuna, halibut, mackerel) to help decrease inflammation
Also be sure to promptly report any new lesions that develop to your doctor, as well as any changes in long-standing lesions.
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
Lupus Foundation of America, 800.558.0121, http://www.lupus.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Keloids
|
| Your doctor has determined that you have one or more keloid scars, or keloids, which are raised nodules of excess scar tissue that form after a skin injury. They are not cancer and do not increase the risk of developing skin cancer. Keloids occur at about the same rate in men and women, and most frequently in darker-skinned individuals such as African-Americans and Asians. The condition usually affects people between the ages of 10 and 30 but can happen at any age. The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. A keloid occurs when the body produces an overgrowth of scar tissue that extends into unaffected areas after an injury or trauma to the skin. Insect bites, acne and chickenpox can also be keloid triggers. The excess tissue usually grows slowly over a period of months to a year or longer, reaching well beyond the original scar and forming a mass. Keloids are reddish when they first develop and become brownish-red then pale over time. Symptoms may include itchiness, tenderness, burning or pain. The texture of a keloid can range from doughy and soft to hard and rubbery. Most are round, oval or oblong. Some may have a claw-like appearance and more irregular borders. The most common locations for keloids are the face, chest, neck, shoulders, back, abdomen and ears, where they can form after ear piercing. Generally keloids do not go away without treatment and can come back after being removed. A keloid may also cause a contracture, or permanent shortening of the scar tissue, which can restrict movement if it overlays a joint or result in serious disfigurement. The tendency to develop keloids often runs in families, likely because of a genetic component. |
Keloids can be treated in a variety of ways depending on factors such as nodule size, depth and location and your age, general health condition and personal preferences. Sometimes more than one treatment may be used at the same time. The following treatment possibilities are available:
Cryosurgery – This treatment method uses super-cooled gas to freeze and flatten keloids, and is often performed in combination with corticosteroid or interferon injections.
Excision – Cutting off keloids with a scalpel is another treatment option. It is most effective when combined with corticosteroid or interferon injections, compression therapy or radiation.
Laser Therapy – A high-intensity light, or laser, can be used to flatten keloids. Laser therapy is sometimes given in combination with corticosteroid injections.
Radiation Therapy – Another keloid treatment method is radiation therapy, which uses a high energy X-ray machine to direct radiation at the nodule. Occasionally radiation therapy is delivered internally via small radioactive pellets implanted directly into the skin.
Corticosteroid Injections – One of the most often used treatments to flatten keloids is the injection of corticosteroids directly into the scar tissue.
Occlusive Dressings – Another standard treatment is the use of occlusive dressings, which do not allow moisture loss or access to the air. These may include silicone gel sheets, non-silicone sheets or medicated tape.
Compression Therapy – Mechanical pressure, or compression therapy, has long been employed as an effective treatment for keloids. Among the many devices used are pressure earrings, special stretchy garments and elastic or Lycra bandages.
Interferon Therapy – One of the more recent developments in keloid treatment is the injection of interferon directly into the scar tissue.
Other Therapies – A variety of other therapies are now being used to treat keloids, such as anti-transforming growth factor, verapamil, bleomycin, 5-fluorouracil, retinoic acid and imiquimod.
You should be sure to tell all of your doctors about your history of developing keloid scars. Other steps you can take to lessen their occurrence include:
• Avoiding non-essential surgery and sharp trauma to the skin, such as piercings and tattoos
• Controlling inflammatory acne if you have it
Also be sure to keep all of your follow-up appointments with your doctor.
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Lipomas
|
| Your doctor has determined that you have one or more lipomas, or deposits of fatty tissue under the skin. They are not cancer and do not increase the risk of developing skin cancer. Lipomas can affect people of any age, but usually arise in early adulthood. They tend to occur more often in women than in men.The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Lipomas occur when round or oval lumps of fat cells grow together within a thin capsule of tissue under the skin. These benign, or harmless, tumors range from the size of a walnut or smaller to that of a baseball. The neck, chest, back, forearms and thighs are the most common sites for lipoma development. The texture of a lipoma is usually soft and rubbery. The overlying skin appears normal and is not connected to the tumor, thus it is moveable under the skin. Most people with lipomas have no noticeable symptoms other than the appearance of the lumps. Some may experience mild tenderness. Lipomas can also cause pain if they grow against a nerve. No one knows what causes lipomas to develop, but there is thought to be a genetic, or inherited, component. They are commonly found in overweight people, but losing weight will not shrink or eliminate lipomas. Some people only have one lipoma, while others may develop many. Occasionally lipomas can arise deeper in the body and affect muscles, tendons, internal organs or other bodily tissues. This type of lipoma more often affects men, and is most commonly found in the large muscles of the arms and legs. |
Treatment for lipomas may not be necessary unless they are large, painful or cosmetically undesirable, in which case they can be removed. The following treatment possibilities are available:
Excision – Cutting out lipomas with a scalpel (excision) is one common method of removal. Stitches may be needed, especially for larger lipomas.
Squeeze Technique – For smaller lipomas situated near the surface of the skin, the squeeze technique may be used. During this procedure, the doctor makes a small stab incision and pushes the lipoma out through the opening.
Liposuction – In some cases lipomas can be removed with a suction device through a small incision. This liposuction technique may provide the potential for less scarring.
Lipomas rarely come back after they are removed. If they do return, or if you have any changes in lipomas that were not removed, be sure to promptly report them to your doctor.
To maximize your health and minimize your risk of ever developing skin cancer, you should strive to prevent skin damage from ultraviolet (UV) ray exposure. General steps you can take include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
• Visiting your doctor regularly for skin cancer screenings
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Melanoma
|
| After completing a thorough lab analysis of your recent skin biopsy, a specialized doctor called a pathologist reported a diagnosis of melanoma, the least common but most aggressive form of skin cancer that accounts for just 4% of all skin cancer cases. Although it frequently affects younger people, the overall chance of having melanoma increases with age. Also, men develop the condition more often than women. The skin is the largest organ of the body. Its top layer is the epidermis, which contains three types of cells that can become cancerous: melanocytes, basal cells and squamous cells. The main purpose of the epidermis is to provide protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Melanoma occurs when the melanocytes — cells in the epidermis that give the skin its color — do not develop and die in their normal manner because of damage from long-term ultraviolet (UV) light exposure, usually from the sun. The extra cells that result form a cancerous (malignant) growth, or tumor, which may invade and damage surrounding areas or spread to other locations in the body (metastasize). Tumors are often found on the torso, head, neck, arms and legs, but can affect other areas such as the palms of the hands, soles of the feet and under the nails. Their appearance may vary, but most are black or brown irregular patches or nodules. Occasionally, melanomas may stop producing pigment and appear flesh-toned, pink, purple or red. People with fair skin, blonde or red hair and blue, green or gray eyes are at a higher risk for melanoma, as are those who have a family history of the condition. However, people with darker skin and eyes can also develop this form of skin cancer. Other risk factors include: • Having many or large moles on the skin Cancer that is confined to the epidermis, the uppermost layer of the skin, is the most manageable and curable. If malignant cells extend more deeply into the skin or into surrounding tissues, lymph nodes or other areas of the body, the treatment plan will be more complex and the cancer may not be curable. Many treatment options are available for patients with incurable melanoma to help minimize pain and improve quality of life. Talk with your doctor about your specific stage of cancer. |
Deciding on a treatment plan for your melanoma can depend upon a variety of factors such as your age, general health condition, stage of cancer and personal preferences. Sometimes more than one type of therapy may be used. The following treatment possibilities are available:
Surgery – The main form of treatment for melanoma is surgery, which removes the tumor along with surrounding tissue. In addition, nearby lymph nodes may be biopsied or removed. Stitches or a skin graft is usually required after surgery. In some cases, Moh's micrographic surgery is performed to treat melanoma. During this procedure, a tumor is removed in microscopic sections, one layer at a time. The surgeon examines each section under a microscope to determine if all of the cancer is gone, or if additional layers need to be removed.
Radiation Therapy – Another melanoma treatment method is radiation therapy, which uses a high energy X-ray machine to direct radiation at the tumor. Radiation therapy can be helpful in controlling metastatic melanoma and reducing symptoms.
Chemotherapy – The use of anti-cancer drugs, or chemotherapy, provides a way to slow tumor growth and reduce pain for patients whose cancer has spread. One particular method called isolated limb perfusion is sometimes used to treat melanoma that is located on an arm or leg.
Biologic Therapy – Newer treatment options such as interferon, interleukin and vaccine therapy are used to enhance the immune system's ability to destroy malignant cells and to reduce symptoms.
You may also consider participating in clinical trials. These investigative studies help doctors learn about new treatments and better ways to use established treatments. Talk with your doctor about the possibility of taking part in a clinical trial in your area.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor. Join a cancer support group and talk with your family, friends, clergyperson or counselor as you feel comfortable. Also, be sure to get enough sleep and eat healthy foods every day.
In addition, you should report any changes to your skin promptly to your doctor and take steps to prevent further skin damage and cancer. Avoid sun exposure, especially between 10 a.m. and 4 p.m. when UV rays are the strongest. You should also use SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating.
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
American Cancer Society, 800.227.2345, http://www.cancer.org/
Skin Cancer Foundation, 800.754.6490, http://www.skincancer.org/
The Melanoma Research Foundation, 800.673.1290, http://www.melanoma.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 10.07
Melanoma in Situ
|
| After completing a thorough lab analysis of your recent skin biopsy, a specialized doctor called a pathologist reported a diagnosis of melanoma in situ, which is the earliest stage of melanoma skin cancer. Melanoma is the least common type of skin cancer, accounting for just 4% of cases, but it is the most aggressive form. However, melanoma is generally curable when found and treated in its earliest stage. The skin is the largest organ of the body. Its top layer is the epidermis, which contains three types of cells that can become cancerous: melanocytes, basal cells and squamous cells. The main purpose of the epidermis is to provide protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Melanoma in situ is the initial phase of melanoma skin cancer in which the cancerous, or malignant, cells are confined to epidermis, the uppermost layer of the skin. The term "in situ" refers to the cancer being located "in one site." The condition occurs when the melanocytes — cells that give the skin its color — do not develop and die in their normal manner because of damage from long-term ultraviolet (UV) light exposure, usually from the sun. The extra cells that result form a malignant growth, or tumor. People with fair skin, blonde or red hair and blue, green or gray eyes are at a higher risk for melanoma in situ. However, people who have darker skin and eyes can also develop the condition. Other risk factors for melanoma in situ include: • Having many or large moles on the skin If the cancer grows more deeply into the skin, it is then considered to be invasive cancer rather than in situ. In invasive melanoma, malignant cells may invade and damage surrounding areas or spread to other locations in the body (metastasize). Thus it is important to promptly treat melanoma in situ before it can progress into invasive melanoma. |
The treatment of choice for melanoma in situ is surgical excision, which removes the tumor along with surrounding tissue. Stitches are usually required after the procedure.
In patients who are not good candidates for surgery for various health reasons, other treatment methods may be used such as topical immunotherapy or radiation therapy. Immunotherapy involves the application of a medicated cream (imiquimod) directly onto the skin (topically) to stimulate the body's immune responses to fight the cancer. In radiation therapy, a high energy X-ray machine is used to direct radiation at the tumor.
After treatment, your doctor will likely recommend that you have periodic skin cancer screening exams to monitor your condition.
You can choose to take an active role in your health and well-being. Learn as much as you can about your condition and have a list of questions ready each time you meet with your doctor.
In addition, you should take steps to prevent further skin damage and occurrences of skin cancer, which include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing long sleeves and pants, a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
• Visiting your doctor regularly for skin checks and promptly reporting any changes in your skin
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
American Cancer Society, 800.227.2345, http://www.cancer.org/
Skin Cancer Foundation, 800.754.6490, http://www.skincancer.org/
The Melanoma Research Foundation, 800.673.1290, http://www.melanoma.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 10.07
Moles (Nevi)
|
| Your doctor has determined that you have one or more moles, or nevi, which are very common skin growths that are usually harmless. Although certain types of moles may occasionally develop into skin cancer, the vast majority are not cancerous. Most adults have between 10 and 40 moles, and some have many more. Nearly all moles arise during the first two decades of life, although additional moles may appear between the ages of 20 and 40. T he skin is the largest organ of the body. Its top layer is the epidermis, which contains three types of cells that can become cancerous: melanocytes, basal cells and squamous cells. The main purpose of the epidermis is to provide protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Moles occur when melanocytes — cells that produce melanin pigment, which gives the skin its color — grow in a cluster along with surrounding tissue, forming a flat or raised, pigmented spot on the epidermis. They can develop anywhere on the body, either singly or in a group. Most moles are acquired, which means they develop after birth. In rare cases, moles are present at birth. They are called congenital nevi. The appearance of moles may vary, but they are normally round or oval and no bigger than a pencil eraser. The coloring is usually brown, tan, pink or flesh-toned, but can be blue or black. Moles often darken and enlarge from sun exposure and the hormonal changes that occur during puberty, pregnancy and birth control pill use. These factors may also contribute to the development of new moles. Moles usually fade or disappear over time, and have an average life cycle of 50 years. Some moles will completely disappear or drop off, while others may never lighten or change at all. People who have many moles are considered to be at greater risk for developing melanoma, the least common but most aggressive form of skin cancer. Congenital nevi are also more apt to become cancerous than moles acquired after birth, especially if they are very large. In addition, those with certain types of moles called dysplastic nevi have an increased melanoma risk. Dysplastic nevi are larger than regular moles, irregularly shaped and unevenly colored. They tend to run in families and are more likely to become cancerous than ordinary moles. Not everyone with dysplastic nevi gets melanoma, however. In fact, most moles never become cancerous. |
Moles can be left untreated if they are not causing any problems and cancer is not present. They may be camouflaged with makeup to make them less noticeable, if desired. If a hair grows out of a mole, it can be trimmed back close to the skin surface with scissors or a razor, or permanently removed with electrolysis.
In cases where a mole is suspicious for cancer, gets in the way of shaving, is cosmetically undesirable to the patient or becomes irritated by clothing or other sources of contact, it can be removed by a doctor.
The usual removal method for moles is to cut or shave them off with a scalpel. Stitches may be needed afterward, especially for larger moles. Serial excision may be required to treat very large moles. During this procedure, a mole is cut away a little at a time until the entire growth is removed. After serial excision, a skin graft will likely be needed.
Occasionally moles come back after they are removed. If they do return, or if you develop any new moles or changes in existing moles such as bleeding, itching or a variation in appearance, be sure to promptly report them to your doctor.
To maximize your health and minimize your risk of ever developing skin cancer, you should strive to prevent skin damage from ultraviolet (UV) ray exposure. General steps you can take include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
• Visiting your doctor regularly for skin checks and promptly reporting any changes in your skin
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
American Cancer Society, 800.227.2345, http://www.cancer.org/
Skin Cancer Foundation, 800.754.6490, http://www.skincancer.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 10.07
Molluscum Contagiosum
|
| Your doctor has determined that you have molluscum contagiosum, a common skin disease caused by a virus that is highly contagious. Although anyone can develop the infection, children tend to get it more frequently than adults, who have often built up immunity to the molluscum contagiosum virus. The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Molluscum contagiosum occurs when the molluscum contagiosum virus enters the skin through small breaks in the hair follicles and causes bumpy growths, or papules, to form in the upper skin layers. The papules: • Are small, pearl-like and often indented in the center Molluscum contagiosum is easily spread to other parts of the body by scratching, which often causes papules to form in a line or cluster. It is also easily spread to other people through skin-to-skin contact. Papules are frequently seen on the face, neck, torso, arms and legs, but may occur elsewhere on the body such as the eyelids or genital area. In people who have weakened immune systems, the papules can be widespread and even disfiguring. Complications of molluscum contagiosum may include the persistence, spread or recurrence of papules, as well as secondary bacterial skin infections. |
Deciding on a treatment plan for your molluscum contagiosum can depend upon a variety of factors such as the location of papules and your age, general health condition and personal preferences. Sometimes molluscum papules are left untreated in patients with normal immune systems because they usually go away on their own after several months. Most of the time, however, they are removed by a doctor to prevent spreading and improve the appearance of the skin, which may be accomplished in one of several ways:
Cryosurgery – Cryosurgery uses super-cooled gas to freeze and destroy papules.
Topical Medication – Another treatment method is the application of medicated cream directly onto the skin (topically). The drugs most often used are retinoid creams or gels, immune modifiers and antiviral medications.
Curettage – This procedure uses a curette (sharp scooping instrument) to scrape off papules.
Electrocautery – In electrocautery, an electrified needle is used to destroy molluscum papules.
Laser Therapy – Sometimes a high-intensity light, or laser, is used to treat molluscum contagiosum.
Chemical Peeling – This method destroys papules by using a chemical agent applied to the skin.
New topical antiviral medications to treat molluscum contagiosum may be developed in the future, providing further options for treatment.
To make sure that you do not spread the molluscum contagiosum infection to other parts of your body or to other people, you should take the following steps:
• Avoid scratching or touching papules by putting tape or a bandage over them
• Keep areas of skin where papules were treated clean and protected
• Do not shave any parts of your body where you have papules
• Avoid contact sports and using swimming pools
• Do not share baths or towels with anyone
• Avoid sexual activity if you have papules on the genital region
Also, be sure to tell your doctor if your papules persist or spread, or if any new symptoms arise.
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Seborrheic Keratoses
|
| Your doctor has determined that you have one or more seborrheic keratoses, which are the most common benign, or harmless, skin growths that affect people over the age of 30. They are not cancer and do not increase the risk of developing skin cancer. Almost all adults develop one or a few seborrheic keratoses (SKs) and some may have many, often in clusters. The condition is more likely with advancing age, and the number of growths often increases over the years. The skin is the largest organ of the body. Its top layer is the epidermis, which provides protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Seborrheic keratoses occur when raised, non-contagious growths form on the outer layer of skin. The exact cause is not known, but the tendency to develop SKs seems to be inherited. Sun exposure does not appear to be a factor in their development. The distinguishing feature of seborrheic keratoses is a waxy, pasted-on look reminiscent of warm candle wax stuck to the skin. They are usually brown in color, but can range from white or light tan to black. Their diameter may vary from a fraction of an inch to larger than an inch, and they can grow larger over time. Sometimes small white or black circles, called horn cysts, may appear within the growth itself. When they first arise, seborrheic keratoses usually look like small light brown bumps. As they grow slowly over time, they darken and thicken, forming an uneven, rough, warty surface. SKs typically develop on the chest or back, although they can appear on many other parts of the body including the scalp, face, neck and legs. They often arise during pregnancy, after hormone replacement therapy or in conjunction with other medical conditions. SKs can be confused with other growths such as warts, moles and melanoma skin cancer. Those conditions, however, do not have a pasted-on appearance and differ in the following ways: • Warts are caused by a virus, usually develop more quickly and are not as dark Since very dark seborrheic keratoses can be mistaken for or blend in with melanoma skin cancer, it is a good idea to have them thoroughly checked by a doctor. |
Seborrheic keratoses can be left untreated if they are not causing any problems. In cases where they get in the way of shaving, are cosmetically undesirable, itch or bleed excessively or become irritated by clothing or other sources of contact, they can be removed by a doctor. One of several methods may be used, depending on the size and location of the growth. Sometimes more than one treatment may be used at the same time. The following treatment possibilities are available:
Cryosurgery – The preferred removal method for SKs is cryosurgery, which uses super-cooled gas to freeze and destroy lesions.
Excision – Cutting off seborrheic keratoses with a scalpel (excision) is another treatment that is sometimes used.
Curettage – This procedure uses a curette (sharp scooping instrument) to scrape of SKs.
Electrocautery – In electrocautery, an electrified needed is used to destroy seborrheic keratoses.
Laser Therapy – Sometimes a high-intensity light, or laser, is used to burn off SKs.
Dermabrasion – SKs can also be removed by "sanding" them off, known as dermabrasion.
There is nothing that can be done to prevent the development of seborrheic keratoses, and occasionally they may come back after being removed. If they do return, or if you develop any other changes in your skin, be sure to promptly report them to your doctor. Also, be sure not to scratch or pick at your seborrheic keratoses because the crumbly scale that comes off will recur, and you could cause a skin infection to develop.
To maximize your health and minimize your risk of ever developing skin cancer, you should strive to prevent skin damage from ultraviolet (UV) ray exposure. General steps you can take include:
• Avoiding the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Using SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wearing a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoiding tanning salons and other UV tanning devices
• Visiting your doctor regularly for skin checks and promptly reporting any changes in your skin
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 9.07
Squamous Cell Carcinoma
|
| After completing a thorough lab analysis of your recent skin biopsy, a specialized doctor called a pathologist reported a diagnosis of squamous cell carcinoma, the second most common form of skin cancer. The condition affects more than 250,000 Americans each year. The skin is the largest organ of the body. Its top layer is the epidermis, which contains three types of cells that can become cancerous: melanocytes, basal cells and squamous cells. The main purpose of the epidermis is to provide protection against the environment. The second layer of the skin is the dermis, which supplies blood, oxygen, strength and support. Underneath the dermis is the hypodermis, or subcutaneous fat layer, which provides an ongoing blood supply to the dermis. Squamous cell carcinoma occurs when squamous cells in the epidermis do not develop and die in their normal manner because of damage from long-term ultraviolet (UV) light exposure, usually from the sun. Most squamous cell tumors are found on the face, ears, scalp, neck, hands and arms. People age 40 and older with fair skin, blonde or red hair and blue, green or gray eyes are at an increased risk for the condition, as are those who work or spend much time outdoors. A squamous cell tumor often looks like a scaly patch with an irritated base. It can also appear as a wart-like or elevated, indented growth or a persistent open sore. Squamous cell carcinoma usually grows slowly but can sometimes spread to other parts of the body, so it is important to find and treat it early. People with the condition have about a 30% chance of developing another squamous cell tumor within five years. They are also at a higher risk for developing other types of skin cancer due to their accumulated sun damage. When squamous cell carcinoma is in its early stage and has not spread beyond the epidermis — the uppermost layer of the skin — it is sometimes called Bowen's disease or squamous cell carcinoma in situ. The term "in situ" refers to the cancer being "in one site." Certain conditions can contribute to the development of squamous cell carcinoma such as burns, persistent sores, scars, previous X-ray treatments, exposure to certain chemicals and, most notably, actinic keratoses, which are scaly, rough-textured patches on the skin caused by sun damage. |
The usual treatment for squamous cell carcinoma is removal by a doctor, which may be accomplished in one of several ways depending on factors such as tumor size and location and your age, general health condition and personal preferences. The following treatment possibilities are available:
Cryosurgery – This treatment uses super-cooled gas to freeze and destroy squamous cell tumors.
Topical Medication – Another treatment method is the application of a medicated cream called 5-fluorouracil directly onto the skin (topically) to destroy tumors.
Excision – The traditional form of treatment for squamous cell carcinoma is excision with a scalpel, which removes the tumor along with surrounding tissue. In addition, nearby lymph nodes may be biopsied or removed.
Curettage and Electrocautery – This treatment method uses a curette (sharp scooping instrument) to remove tumors, then an electrified needle to stop the bleeding.
Laser Therapy – Sometimes a high-intensity light, or laser, is used to destroy squamous cell tumors.
Radiation Therapy – Another treatment method is radiation therapy, which uses a high energy X-ray machine to direct radiation at the tumor. It is often favored for cancers in areas that are difficult to treat and for recurrent lesions that were previously treated surgically.
Mohs Micrographic Surgery – Performed by a dermatologic surgeon, this highly specialized procedure has the highest cure rate of all squamous cell carcinoma treatments and provides a minimal amount of tissue removal. During Mohs surgery, a tumor is removed in microscopic sections, one layer at a time. The surgeon examines each section under a microscope to determine if all of the cancer is gone, or if additional layers need to be removed.
Other treatments for squamous cell carcinoma are being studied such as photodynamic therapy, which burns tumors off with a laser after illuminating them with a photosensitizing drug, and biologic therapy, which boosts the immune system's ability to destroy cancer cells.
Your doctor will likely recommend that you have periodic skin cancer screening exams to monitor your condition. In addition to keeping those appointments, you should take the following steps to prevent further skin damage and occurrences of skin cancer:
• Avoid the sun, especially between 10 a.m. and 4 p.m. when UV rays are the strongest
• Use SPF 15 or higher sunscreen that contains avobenzone (Parsol 1789), titanium dioxide and/or zinc oxide, applying it 20 minutes before going outdoors and again every two hours, or immediately after swimming or sweating
• Wear long sleeves and pants, a wide-brimmed hat and 100% UV-blocking sunglasses when outdoors
• Avoid tanning salons and other UV tanning devices
American Academy of Dermatology, 888.462.3376, http://www.aad.org/
American Cancer Society, 800.227.2345, http://www.cancer.org/
This patient resource sheet is provided to you as a service of CBLPath® and is intended for information purposes only. It may not fully describe all aspects of your diagnosis and is not meant to serve as medical advice or a substitute for professional medical care. Your physician can provide you with a thorough explanation of your diagnosis and appropriate treatment options, which may vary. Only you and your physician can determine your best treatment plan.
Updated 10.07

